Sleep Aid Risk Calculator
How Sleep Aids May Affect Your Brain
This calculator helps you understand your personal risk based on factors discussed in the article. It's not a substitute for medical advice, but it can help you have a more informed conversation with your doctor.
Risk Assessment
Low Risk
Recommendation: Continue monitoring but consider discussing with your doctor if you have any concerns. You may want to explore non-pharmaceutical approaches like sleep hygiene or CBT-I for long-term sleep improvement.
More than 4 million older Americans take sleep aids every year. Many do so without realizing how deeply these pills can mess with their thinking, memory, and daily focus. It’s not just about feeling groggy in the morning. Some sleep medications are quietly increasing the risk of memory loss, confusion, and even dementia - especially in people over 65. But not all sleep aids are the same. Some might even help protect your brain. The truth is messy, complicated, and full of contradictions. And if you’re taking one right now, you need to know the real risks - and the safer alternatives.
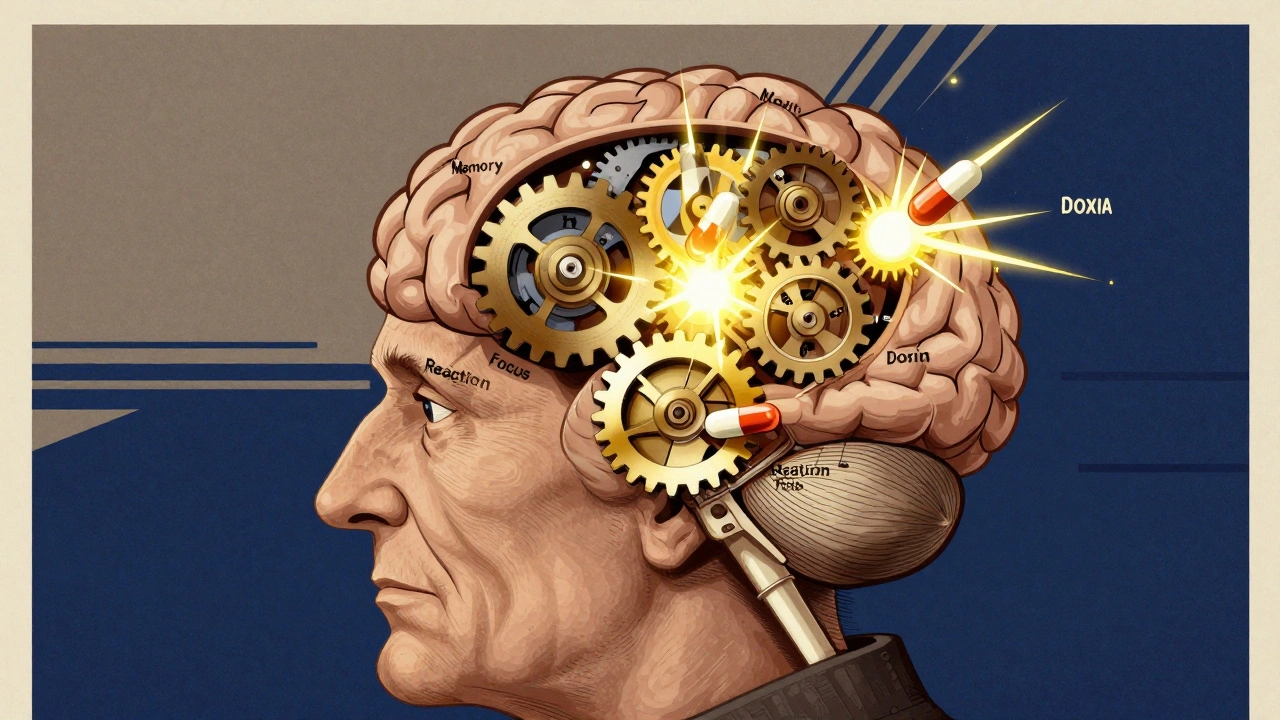
What Sleep Aids Are Actually Doing to Your Brain
Most prescription sleep pills work by flooding your brain with calming chemicals. Benzodiazepines like lorazepam and non-benzodiazepine hypnotics like zolpidem (Ambien) target GABA receptors - the brain’s main brake pedal. This slows down neural activity, making you drowsy. But here’s the problem: GABA receptors are everywhere. They’re involved in memory formation, attention, and reaction time. When you hit them hard with a pill, you don’t just turn off sleeplessness - you also turn down your mental clarity.
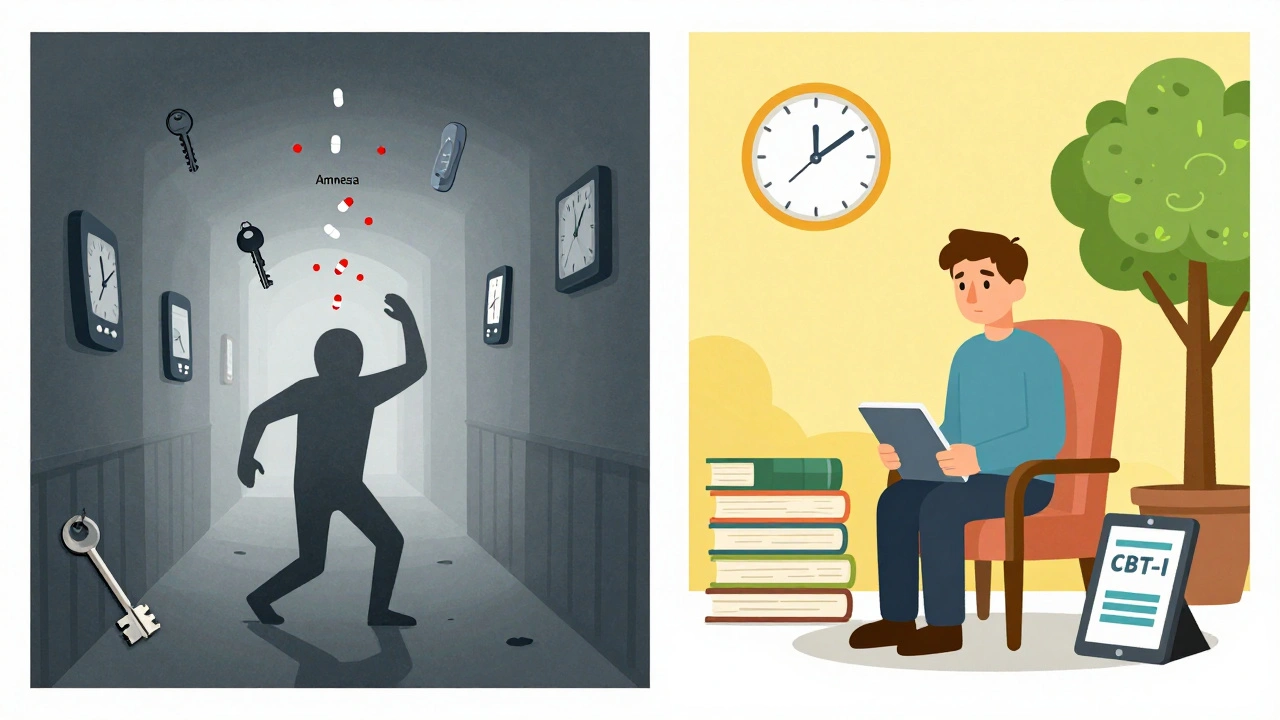
Studies show people on these drugs have up to a 20% drop in cognitive test accuracy. Reaction times slow. Short-term memory falters. In one trial with monkeys, those given high doses of GABA-boosting drugs performed worse on learning tasks than those given a placebo. In humans, this shows up as next-day brain fog, trouble concentrating, or even memory lapses during the night. Reddit users report waking up with no memory of walking to the kitchen or checking their phone. One in four people taking zolpidem say they’ve had full-blown amnesia episodes - not just forgetting where they put their keys, but forgetting entire chunks of the night.
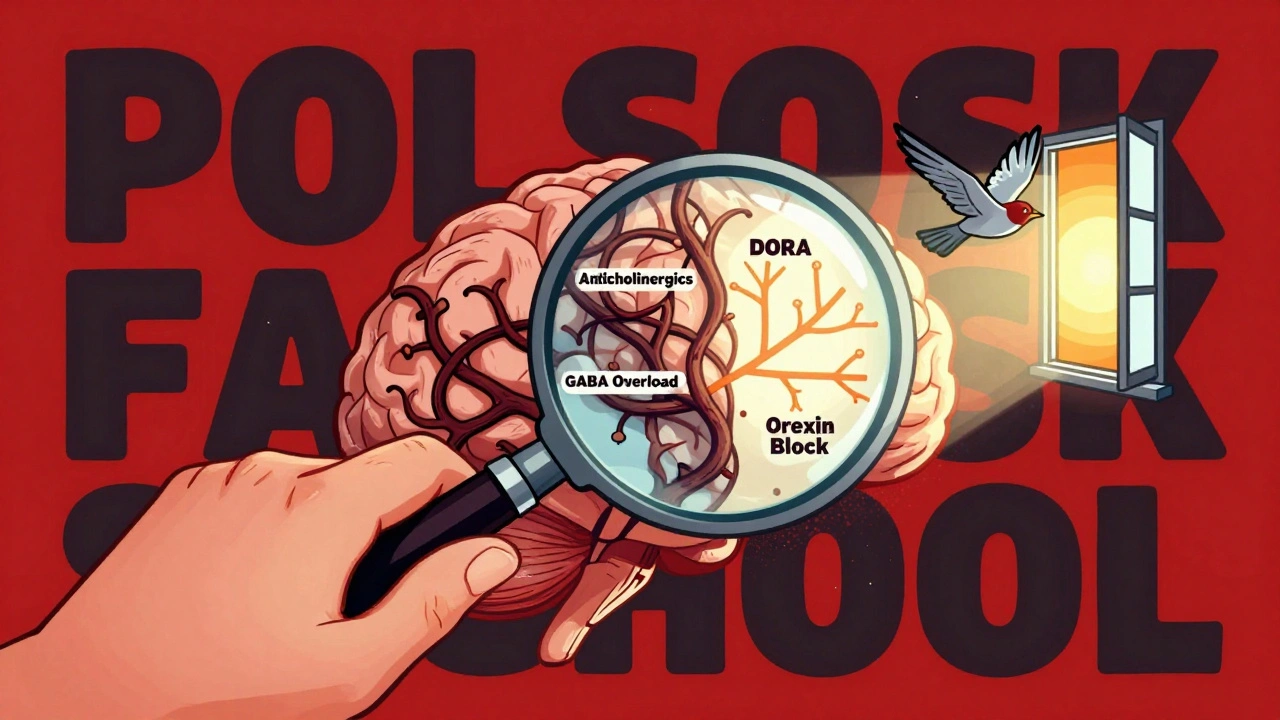
The Anticholinergic Trap
Then there’s trazodone - often prescribed off-label as a sleep aid because it’s cheap and seems gentle. But trazodone, along with many older antidepressants and antihistamines, is an anticholinergic. These drugs block acetylcholine, a key neurotransmitter for learning and memory. The link between anticholinergics and cognitive decline isn’t theoretical. A landmark 2010 study from Indiana University tracked thousands of older adults and found a direct connection: those taking these drugs were significantly more likely to develop mild cognitive impairment - the early warning sign of dementia.
What’s scary is how common this is. Many people don’t realize their allergy medicine, bladder control pill, or even over-the-counter sleep aid contains anticholinergics. Dr. Malaz Boustani, who led that study, puts it bluntly: “Something as seemingly benign as a medication for sleep or motion sickness can cause or worsen cognitive impairment.” The good news? This kind of impairment may be reversible if you stop the drug. The bad news? Most people don’t connect their brain fog to their nightly pill.
The DORA Revolution: A New Hope?
Not all sleep aids are created equal. A new class called dual orexin receptor antagonists (DORAs) - like suvorexant (Belsomra) and daridorexant (Quviviq) - works completely differently. Instead of suppressing brain activity broadly, they block orexin, the brain’s wakefulness signal. Think of it like turning off a light switch instead of drowning the room in sedatives.
Early research is promising. In a small 2023 study from Washington University, people taking suvorexant showed lower levels of amyloid-beta and tau - two proteins that build up in Alzheimer’s disease. That’s huge. It suggests this class might not just help you sleep, but actually protect your brain. Animal studies of DORA-22, still in testing, showed no cognitive side effects at all - while still improving sleep. Users on Drugs.com report fewer morning grogginess complaints with suvorexant than with zolpidem. Sixty-two percent gave it 4 or 5 stars, citing “clearer mornings” and “no brain fog.”
But here’s the catch: this doesn’t mean you should start taking suvorexant to prevent dementia. The study was short-term, involved only a few dozen people, and didn’t prove long-term protection. Dr. Brendan Lucey, who led the research, warns: “It’s encouraging, but premature to say this is a dementia-prevention drug.” Still, for people who need medication, DORAs are currently the safest bet.
Who’s at the Highest Risk?
Age matters - a lot. The American Geriatrics Society’s Beers Criteria, updated in 2023, says people over 65 should avoid benzodiazepines, zolpidem, and tricyclic antidepressants entirely. Why? Because aging brains are more sensitive. Metabolism slows. Drug levels build up. The same dose that helps a 40-year-old sleep can leave an 80-year-old confused and unsteady.
Race also plays a role - and it’s unsettling. A nine-year study of 3,000 older adults found white participants who used sleep meds frequently had a 79% higher risk of dementia. Black participants? No increased risk. Researchers aren’t sure why. Could be genetics. Could be differences in medication dosing. Could be access to care. Whatever the reason, it’s a stark reminder that blanket advice doesn’t work.
And then there’s duration. Taking a sleep aid for two nights? Probably fine. Taking it every night for six months? That’s when the risks climb. A 2021 study found routine users had a 30% higher chance of developing dementia over time. But zolpidem and trazodone? Those two didn’t show the same link in a 2019 NIH study of over 3,000 people. So even within the same category, some drugs are safer than others.
The Real Cost of Sleeping Pills
It’s not just about dementia. Sleep aids increase your risk of falls, car crashes, and hip fractures - especially in older adults. One study found people on zolpidem were 60% more likely to be in a motor vehicle accident. The FDA added stronger warning labels to these drugs in 2022, but most patients never read them.
And the dependency is real. Stopping suddenly can trigger rebound insomnia - worse than before you started. Anxiety, sweating, even seizures can happen. That’s why doctors recommend tapering off slowly over 4 to 8 weeks. But most people just quit cold turkey because the side effects feel unbearable. They’re stuck between a rock and a hard place.
What Actually Works Better
There’s a better path - and it doesn’t involve pills. Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s not a quick fix. You need 6 to 8 weekly sessions with a trained therapist. But the results last. Unlike pills, CBT-I rewires your brain’s sleep patterns. You learn to associate your bed with sleep, not stress. You fix bad habits like lying awake for hours or checking the clock. Digital versions like Sleepio cost $300-$500 and have been shown to work just as well as in-person therapy.
And it’s working. In 2015, only 12% of primary care providers recommended CBT-I first. By 2023, that number jumped to 47%. The American College of Physicians now says CBT-I should be the first-line treatment for chronic insomnia - not medication. The American Academy of Sleep Medicine lists over 1,200 certified CBT-I providers. The National Sleep Foundation offers free tools and guides used by millions.
It takes longer to see results - two to three weeks versus one night. But you won’t wake up confused. You won’t risk memory loss. You’ll sleep better, longer, and without chemicals.
What You Should Do Right Now
If you’re on a sleep aid and you’re over 65, talk to your doctor. Don’t stop cold turkey. Ask: Is this a benzodiazepine? Is it anticholinergic? Is there a DORA alternative? If you’re on zolpidem or trazodone, ask if you really need it. The NIH study suggests these might be safer than others - but that doesn’t mean they’re risk-free.
If you’ve been taking sleep meds for more than a few months, consider CBT-I. It’s not magic. It takes effort. But it’s the only treatment proven to improve sleep without harming your brain.
And if you’re thinking about starting a sleep aid? Don’t. Try sleep hygiene first. Keep a consistent schedule. Avoid screens before bed. Get sunlight in the morning. Limit caffeine after noon. Most insomnia isn’t caused by broken biology - it’s caused by bad habits. Fix those first.
The pills might feel like a lifeline. But they’re a temporary fix with long-term costs. Your brain doesn’t need more chemicals. It needs rest, routine, and safety. Those are free. And they work.
Do sleep aids cause dementia?
Some do, but not all. Benzodiazepines, anticholinergics, and long-term use of GABA-modulating drugs like zolpidem are linked to higher dementia risk - especially in older adults. But newer drugs called DORAs, like suvorexant, show no cognitive harm and may even reduce Alzheimer’s-related brain proteins. The risk depends on the drug, your age, and how long you take it.
Is trazodone safe for sleep?
Trazodone is often used off-label for sleep, but it’s an anticholinergic - a class of drugs linked to memory problems and mild cognitive impairment. While a 2019 NIH study found no direct link to dementia in older adults, it still carries cognitive risks. For people over 65, safer alternatives like CBT-I or DORAs are preferred. Don’t assume it’s harmless just because it’s not a “sleep pill.”
What’s the safest sleep aid for seniors?
The safest option isn’t a pill - it’s CBT-I. If medication is absolutely necessary, DORAs like suvorexant or daridorexant are currently the best choices because they don’t impair cognition and don’t cause dependence. Avoid benzodiazepines, zolpidem, and trazodone if you’re over 65. The American Geriatrics Society explicitly advises against them.
Can I stop taking sleep aids cold turkey?
No. Stopping benzodiazepines or zolpidem suddenly can cause rebound insomnia, anxiety, tremors, or even seizures. Always taper off slowly under medical supervision - usually over 4 to 8 weeks. Your doctor can help you switch to a safer alternative or begin CBT-I while reducing your dose.
How long does it take for CBT-I to work?
Most people start seeing improvements in 2 to 3 weeks. Full benefits usually take 6 to 8 weeks of consistent work. Unlike pills that work in hours, CBT-I rewires your brain’s sleep habits. It takes time, but the results last - without side effects or dependency.
Are over-the-counter sleep aids safe?
Most OTC sleep aids contain antihistamines like diphenhydramine or doxylamine - both are strong anticholinergics. They’re linked to memory problems, confusion, and increased dementia risk, especially in older adults. Don’t assume “natural” or “non-prescription” means safe. They’re just as risky as prescription pills for long-term use.
Next Steps If You’re Worried
Start by listing every medication you take - including OTC pills, supplements, and nighttime remedies. Look up each one for anticholinergic or GABA-modulating effects. If you’re on anything from the Beers Criteria list, talk to your doctor this week.
Visit the American Academy of Sleep Medicine’s website and search for a CBT-I provider near you. Many offer virtual sessions. Try Sleepio or similar apps if you can’t find a therapist. Give it 4 weeks. Track your sleep and your mental clarity. You might be surprised at how much better you feel without pills.
And if you’re still unsure? Don’t guess. Ask. Your brain is worth more than a quick fix.