One glass of grapefruit juice in the morning might seem like a healthy habit-until it starts messing with your meds. For millions of people taking prescription drugs, this citrus fruit isn’t just a breakfast sidekick; it’s a silent risk. The problem isn’t about sugar or acidity. It’s about chemistry. Grapefruit contains compounds that can turn safe doses of medication into dangerous ones, sometimes with life-threatening results.
Why Grapefruit Changes How Your Drugs Work
It all starts in your gut. When you drink grapefruit juice, chemicals called furanocoumarins-mainly bergamottin and 6',7'-dihydroxybergamottin-hit the lining of your small intestine. There, they disable an enzyme called CYP3A4. This enzyme normally breaks down many drugs before they enter your bloodstream, acting like a filter. When it’s shut down, the drug slips through untouched. That means your body absorbs way more than it should.
Unlike caffeine or alcohol, where timing matters (wait a few hours, and the effect fades), grapefruit’s damage lasts for days. Once CYP3A4 is blocked, your body has to make new enzymes to replace them. That takes 24 to 72 hours. So even if you take your pill at night and drink juice in the morning, you’re still at risk. There’s no safe window. The only reliable fix? Avoid grapefruit entirely while on these drugs.
Statins: The Most Common and Dangerous Interaction
Statins are among the most prescribed drugs in the world-used to lower cholesterol and prevent heart attacks. But not all statins react the same way to grapefruit.
- Simvastatin (Zocor): A single 200-milliliter glass of grapefruit juice can triple your blood levels. That pushes you from a safe 15 ng/mL to 45 ng/mL or higher, massively increasing the chance of muscle breakdown (rhabdomyolysis), kidney failure, and even death.
- Lovastatin (Mevacor): Bioavailability can jump by 1,500%. That’s not a typo. One study showed levels spiked so high that patients needed emergency care.
- Atorvastatin (Lipitor): Blood levels rise by about 80%. Still risky, but less extreme than the others.
- Pravastatin (Pravachol) and Rosuvastatin (Crestor): These are safe. They don’t rely on CYP3A4 for metabolism. If you love grapefruit and need a statin, these are your best options.
Doctors often switch patients from simvastatin to rosuvastatin just to avoid this interaction. It’s not about cost or effectiveness-it’s about safety.
Calcium Channel Blockers: Blood Pressure Meds That Can Turn Deadly
If you’re on blood pressure medication, grapefruit could be quietly raising your risk of fainting, dizziness, or heart rhythm problems.
- Felodipine (Plendil): The drug that started it all. In the original 1989 study, grapefruit juice boosted felodipine levels by 355%. That’s enough to cause dangerously low blood pressure.
- Nifedipine (Procardia, Adalat CC): Blood levels increase by 274%. Even the extended-release version isn’t safe.
- Amlodipine (Norvasc): Levels rise by 150%. While less dramatic than others, the risk is still real, especially in older adults.
These drugs are often taken daily. Combine that with a daily glass of grapefruit juice, and you’re stacking risk on top of routine. Many patients don’t realize they’re doing something dangerous because their doctor never mentioned it.

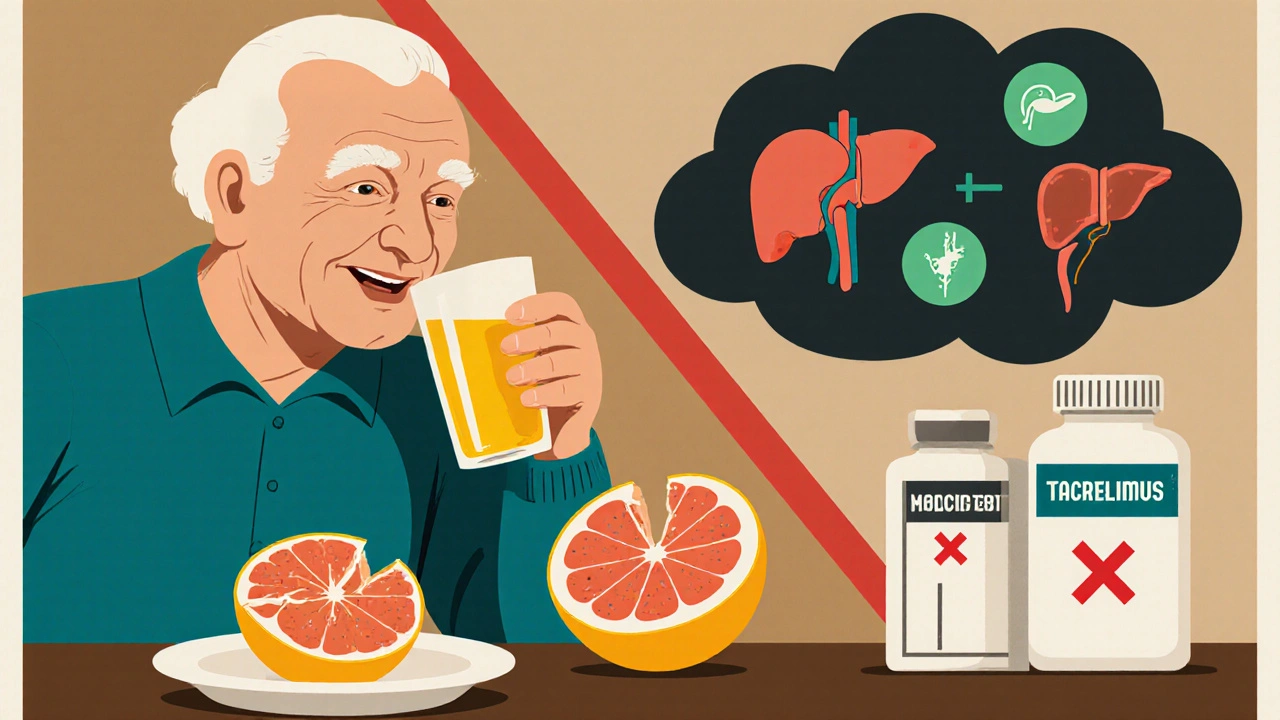
Immunosuppressants: A Recipe for Organ Rejection or Infection
If you’ve had a transplant, grapefruit could be the reason your body starts rejecting the new organ-or why you get a deadly infection.
- Cyclosporine (Sandimmune, Neoral): Blood levels rise by 50-60%. Too much means kidney damage, high blood pressure, and tremors.
- Tacrolimus (Prograf, Envarsus XR): Levels can spike 300-500%. This isn’t just risky-it’s life-threatening. Patients have been hospitalized for kidney failure after just one week of grapefruit juice.
- Sirolimus (Rapamune): AUC increases by 1,100%. That’s more than ten times the normal amount in your blood.
These drugs are tightly monitored with regular blood tests. But even if your levels look fine one week, a single glass of grapefruit juice the next day can throw everything off. Transplant centers now include grapefruit avoidance in their patient handbooks-and for good reason.
Other High-Risk Medications
The list goes on. The FDA has flagged 17 prescription drugs with mandatory grapefruit warnings. Here are a few more:
- Buspirone (Buspar): Used for anxiety. Grapefruit can cause extreme drowsiness and low blood pressure.
- Sildenafil (Viagra): Grapefruit can double its effect, leading to dangerous drops in blood pressure.
- Colchicine (Colcrys): Used for gout. Too much can cause muscle damage and organ failure.
- Quetiapine (Seroquel): An antipsychotic. Grapefruit can cause sedation, dizziness, and heart rhythm issues.
And it’s not just juice. Whole grapefruit, grapefruit extracts, and even some flavored waters or candies with grapefruit flavoring can trigger the reaction. Always check labels.
What About Other Citrus Fruits?
Not all citrus is safe. Seville oranges (used in marmalade), pomelos, and some limes contain the same furanocoumarins. If your orange juice says “bitter orange” or “Seville orange,” avoid it. Regular sweet oranges (like Valencia or Navel) and lemons are fine. They don’t contain these compounds.
Even pomegranate juice has been linked to similar interactions in rare cases. If you’re on a high-risk medication, it’s safer to skip it until you check with your doctor.
What Should You Do?
If you take any prescription drug, here’s what to do:
- Ask your doctor or pharmacist: “Does my medication interact with grapefruit?” Don’t assume it’s safe just because you’ve been drinking it for years.
- Check your pill bottle: Look for warnings on the label or patient information sheet. If it says “avoid grapefruit,” take it seriously.
- Know your alternatives: For statins, switch to pravastatin or rosuvastatin. For blood pressure, ask about diltiazem or lisinopril instead of amlodipine. For immunosuppressants, your doctor may adjust the dose or switch you to a non-interacting drug.
- Don’t rely on timing: Waiting 4 hours between juice and pills won’t help. The enzyme stays blocked for days.
- Be honest: If you love grapefruit and don’t want to quit, tell your doctor. They can find a safe alternative.
Pharmacists are trained to catch these interactions. In 2022, nearly 80% of community pharmacists routinely screened for grapefruit-drug interactions during medication reviews. Don’t be shy-ask them.
Why This Matters More Than Ever
More than half of Americans over 65 take five or more prescriptions. That’s a huge group at risk. The CDC says 52.3% of older adults are on multiple meds. Many of those drugs interact with grapefruit. At the same time, 42.7% of seniors eat grapefruit at least once a week, according to national nutrition surveys.
That’s not a coincidence. It’s a public health problem. The FDA estimates grapefruit interactions cause about 10,000 adverse events each year in the U.S. alone. Hospitals now have electronic alerts built into their systems to warn doctors when a patient is prescribed a risky drug and has a history of grapefruit use.
And it’s not going away. The elderly population is growing fast. By 2040, over 80 million Americans will be 65 or older. More meds. More grapefruit. More danger.
Final Thought: It’s Not About Fear-It’s About Control
You don’t have to give up healthy eating. You just need to know what’s safe. Grapefruit isn’t evil. It’s full of vitamin C and antioxidants. But for some people, it’s a hidden danger. The good news? You have power here. Ask questions. Know your meds. Talk to your pharmacist. Swap out a risky drug for a safe one. You can still enjoy your morning routine-just make sure it doesn’t cost you your health.
Can I drink grapefruit juice if I take a low dose of my medication?
No. Even a small amount of grapefruit juice-like half a glass-can block the CYP3A4 enzyme enough to cause dangerous drug buildup. The effect isn’t about dose; it’s about enzyme inhibition. Once blocked, your body can’t clear the drug properly, no matter how little you take.
How long should I wait after drinking grapefruit juice before taking my medication?
You can’t wait it out. The enzyme inhibition lasts 24 to 72 hours. Even if you drink grapefruit juice at breakfast and take your pill at bedtime, the interaction still happens. The only safe option is to avoid grapefruit completely while on the medication.
Are all grapefruit products the same? What about grapefruit extract or flavored water?
Yes, they’re all risky. Grapefruit extract, flavored teas, candies, and even some salad dressings with grapefruit oil contain the same furanocoumarins. Always read ingredient labels. If it says “grapefruit,” “citrus paradisi,” or “natural grapefruit flavor,” assume it’s unsafe unless your doctor says otherwise.
Can I switch to orange juice instead?
Yes, sweet oranges like Valencia or Navel are safe. They don’t contain furanocoumarins. But avoid Seville oranges (bitter oranges), pomelos, and limes. Stick to regular orange juice, apple juice, or water if you’re unsure.
What if I accidentally drank grapefruit juice while on a risky medication?
If you’re on a high-risk drug like simvastatin, cyclosporine, or tacrolimus, watch for symptoms: unexplained muscle pain, weakness, dark urine, dizziness, or irregular heartbeat. Call your doctor right away. You may need blood tests to check for organ damage. Going forward, avoid grapefruit completely.
Are there any new medications that don’t interact with grapefruit?
Yes. Newer drugs are often designed to avoid CYP3A4 metabolism. For example, rosuvastatin and pravastatin don’t interact, unlike older statins. Newer blood pressure drugs like lisinopril or valsartan are also safe. When possible, your doctor can choose these alternatives to reduce risk.
