When someone is diagnosed with type 1 diabetes, it’s not just about high blood sugar-it’s about the immune system turning against the pancreas. This isn’t a lifestyle issue. It’s not caused by eating too much sugar. It’s an autoimmune war inside the body, where the immune system attacks and kills the insulin-producing beta cells in the pancreas. Once those cells are gone, the body can’t make insulin anymore. And without insulin, glucose can’t enter cells for energy. The result? Blood sugar spikes, fatigue, weight loss, and if left untreated, life-threatening complications.
How Type 1 Diabetes Starts: The Autoimmune Trigger
Type 1 diabetes begins long before symptoms show. Years before a child or adult feels thirsty, loses weight, or gets diagnosed, the immune system starts making autoantibodies. These are like faulty missiles targeting specific proteins on pancreatic beta cells: insulin itself, GAD65, IA-2, and ZnT8. These autoantibodies don’t cause damage directly, but they signal that immune cells-especially T-cells-are already inside the pancreas, attacking the insulin factories. This process is called insulitis. It’s not random. Genetics play a big role. People with HLA-DR3 or HLA-DR4 gene variants have a 20 to 30 times higher risk. But genes alone don’t explain why one person gets it and another doesn’t. Environmental triggers matter. Enteroviruses, like coxsackievirus B, are strongly linked. Studies show people who later develop type 1 diabetes often had viral infections months before diagnosis. Other suspects include vitamin D deficiency, early exposure to cow’s milk, and gut bacteria imbalances. One 2022 study found that people with type 1 diabetes have less of a gut bacterium called Faecalibacterium prausnitzii-a key producer of butyrate, which helps calm inflammation.The Three Stages of Type 1 Diabetes
Type 1 diabetes doesn’t happen overnight. Scientists now recognize three clear stages:- Stage 1: Two or more autoantibodies are present, but blood sugar is still normal. About 0.4% of the general population is here-often unaware.
- Stage 2: Blood sugar starts to rise, but the person still feels fine. This is the window where intervention might work.
- Stage 3: Symptoms appear-frequent urination, extreme thirst, weight loss, fatigue. By this point, most beta cells are already destroyed, and insulin therapy is mandatory.
Insulin Is Not Optional
Unlike type 2 diabetes, where the body still makes some insulin but doesn’t use it well, type 1 diabetes means the body makes almost none. At diagnosis, C-peptide levels-a marker of natural insulin production-are usually below 0.2 nmol/L. Healthy people have over 0.6. That’s why insulin therapy isn’t a choice. It’s survival. Today’s standard is multiple daily injections (MDI) or insulin pumps. MDI means taking a long-acting insulin (like glargine U-300) once a day for background needs, plus rapid-acting insulin (like aspart or lispro) before meals. Pumps deliver insulin continuously and can be programmed to adjust based on meals or activity. But insulin alone isn’t enough. Blood sugar targets have gotten tighter. The American Diabetes Association recommends keeping blood glucose between 80-130 mg/dL before meals and under 180 mg/dL after meals. The goal? An A1c under 7%. But for many, especially kids, the target is even lower-6.5%-to protect long-term health.
Technology Is Changing the Game
The biggest leap in type 1 diabetes care isn’t a new drug-it’s technology. Continuous glucose monitors (CGMs), like the Dexcom G7, track blood sugar every 5 minutes without fingersticks. They alert users when levels are dropping too low or rising too fast. The 2023 DIAMOND trial showed CGMs lowered A1c by 0.4-0.6% and cut hypoglycemic events by half. Even better are closed-loop systems-sometimes called artificial pancreases. Devices like Tandem’s Control-IQ use algorithms to automatically adjust insulin delivery based on real-time CGM data. In a 2022 JAMA study, users spent 71-74% of the day in the target range (70-180 mg/dL). Without the system, it was just 51-55%. For parents of kids with type 1, this isn’t convenience-it’s peace of mind.When the Pancreas Attacks Itself-Beyond Beta Cells
Most people think type 1 diabetes only affects the endocrine pancreas-the part that makes insulin. But sometimes, the autoimmune attack spreads. A rare condition called autoimmune pancreatitis (AIP) can happen alongside type 1 diabetes. In AIP, the immune system attacks the exocrine pancreas-the part that makes digestive enzymes. This leads to abdominal pain, bloating, and poor digestion. This combo happens in about 0.3% of type 1 cases, but it’s critical to recognize. AIP is often diagnosed by elevated IgG4 levels, specific imaging, or biopsy. Treatment? Corticosteroids. But here’s the catch: steroids raise blood sugar. So if a type 1 patient gets AIP, their insulin doses often need to be doubled or tripled temporarily. It’s a double burden: managing two autoimmune diseases at once. That’s why the ADA now recommends checking for pancreatic enzyme deficiency in type 1 patients with ongoing digestive issues. About 5-10% of long-term type 1 patients develop this. They need enzyme supplements like Creon to digest food properly.Emerging Therapies: Beyond Insulin
The future of type 1 diabetes isn’t just better insulin-it’s stopping the immune attack and saving what’s left of the pancreas. Teplizumab is just the beginning. Trials are underway with drugs like abatacept, which blocks T-cell activation. One 2023 study showed it cut C-peptide decline by 59% in people recently diagnosed. Verapamil, a blood pressure drug, showed surprising results in a 2022 trial: it preserved 30% more insulin production over 12 months. Why? It may reduce beta-cell stress, which seems to trigger the immune attack. The most exciting breakthrough? Stem cell-derived islet cells. Vertex Pharmaceuticals’ VX-880 therapy implants lab-grown beta cells into patients. In a 2023 NEJM trial, 89% of the 12 participants became insulin-independent after 90 days. One patient stopped all insulin and stayed off it for over a year. This isn’t science fiction-it’s happening now.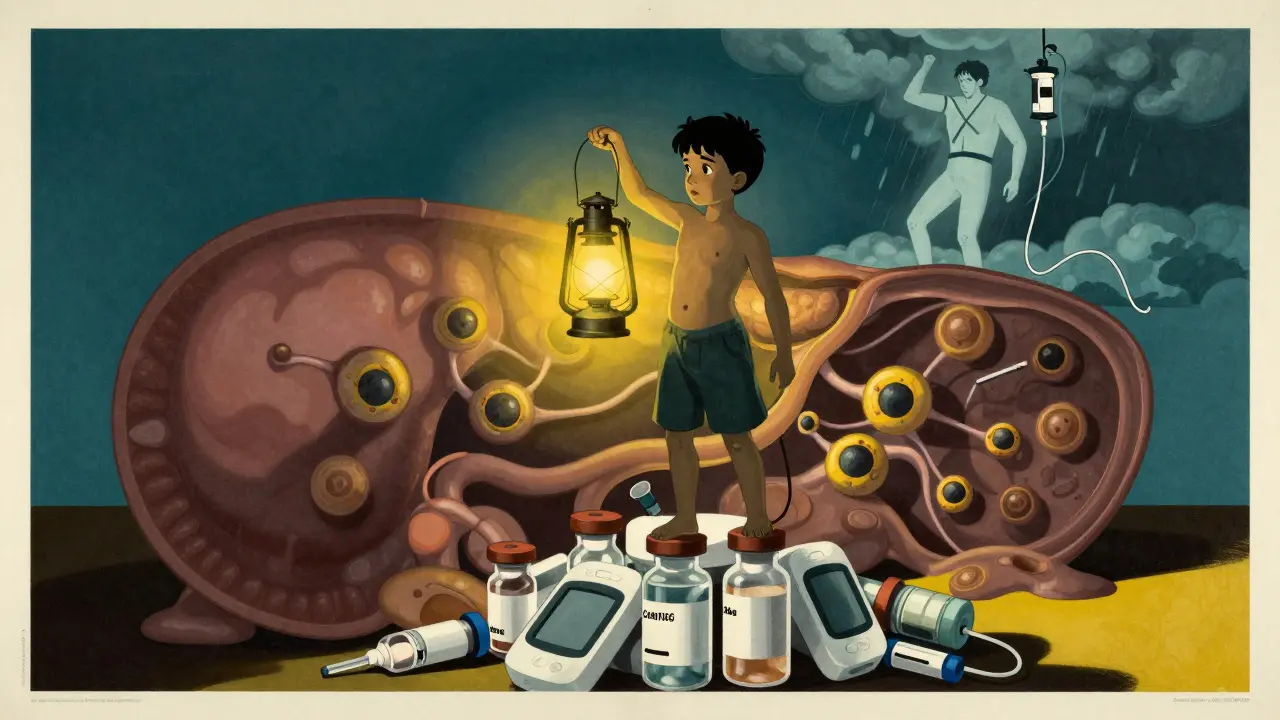
Cost, Access, and the Real Burden
Despite all the progress, type 1 diabetes remains expensive and hard to manage. In the U.S., annual costs average $19,743 per person. Insulin alone makes up nearly $10,000 of that. Even with insurance, many still ration insulin because of high copays. This isn’t theoretical-people die because they can’t afford their medication. Globally, type 1 diabetes affects about 8.7 million people. In children under 14, incidence is rising by 3-4% each year. The disease doesn’t discriminate by income, race, or geography. But access to technology, education, and care does.What Comes Next?
The future of type 1 diabetes management is combination therapy: immunotherapy to stop the attack, plus beta-cell protectors to save what’s left, plus advanced delivery systems to keep blood sugar stable. The 2024 ADA/EASD guidelines already call this the next frontier. For now, the best strategy is early detection, tight control, and using every tool available. CGMs, pumps, insulin analogs, and now teplizumab are giving people with type 1 diabetes more time, more stability, and more hope.Frequently Asked Questions
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes is an autoimmune attack on the insulin-producing beta cells in the pancreas (endocrine function). Autoimmune pancreatitis (AIP) attacks the enzyme-producing parts of the pancreas (exocrine function). They are separate conditions, but they can occur together in rare cases-about 1 in 300 people with type 1 diabetes. When they do, treatment requires both insulin and corticosteroids, with careful monitoring of blood sugar because steroids raise glucose levels.
Can type 1 diabetes be reversed?
Not yet. Once beta cells are destroyed, they don’t regenerate on their own. But new treatments can slow or even pause the process. Teplizumab can delay diagnosis by over two years in people at Stage 2. Stem cell therapies like VX-880 have restored insulin production in some patients, allowing them to stop insulin injections. These aren’t cures, but they’re the closest we’ve ever come.
Why do some adults get diagnosed with type 1 diabetes later in life?
This is called LADA-Latent Autoimmune Diabetes in Adults. It’s still type 1 diabetes, but the immune attack is slower. People with LADA may produce a little insulin for years after diagnosis, so they’re often misdiagnosed as type 2. About 12% of adults diagnosed with type 2 actually have LADA. Testing for autoantibodies and C-peptide levels can clarify the diagnosis. LADA patients eventually need insulin, but not always right away.
What’s the difference between insulin analogs and human insulin?
Human insulin is a copy of the insulin your body naturally makes. Insulin analogs are slightly modified versions designed to act faster or last longer. Rapid-acting analogs (like aspart or lispro) start working in 10-15 minutes and peak in 1-2 hours, matching meals better. Long-acting analogs (like glargine U-300) provide steady coverage for up to 36 hours with less risk of nighttime lows. They’re more expensive, but studies show they reduce hypoglycemia by 20-30% compared to older human insulins.
Can diet or fasting cure type 1 diabetes?
No. While diet helps manage blood sugar, it cannot restore lost beta cells or stop the autoimmune attack. Some people with type 1 diabetes report feeling better on low-carb diets, and research is exploring how gut health affects disease progression. But no diet, supplement, or fasting protocol has ever reversed type 1 diabetes. Relying on these instead of insulin is dangerous and can lead to diabetic ketoacidosis-a medical emergency.
How do I know if I’m at risk for type 1 diabetes?
If you have a close relative with type 1 diabetes, your risk is higher. Screening for autoantibodies (GAD65, IA-2, ZnT8, insulin autoantibodies) is available through research programs like TrialNet. Even if you feel fine, having two or more autoantibodies means you’re in Stage 1 or 2. Early detection opens the door to interventions like teplizumab that can delay or prevent full-blown diabetes.
