Many people take turmeric for its anti-inflammatory benefits, believing it’s just a harmless spice. But if you’re on a blood thinner like warfarin, aspirin, or rivaroxaban, turmeric could be putting you at serious risk - not because it’s toxic, but because it acts like a second blood thinner inside your body. And unlike prescription drugs, turmeric supplements don’t come with dosage labels, safety warnings, or monitoring protocols. The result? A quiet, growing danger that’s already landed people in emergency rooms.
How Turmeric Actually Thins Your Blood
Turmeric gets its color and most of its power from curcumin, a compound that makes up only 2-8% of raw turmeric root but can be as high as 95% in concentrated supplements. Curcumin doesn’t just reduce swelling or ease joint pain - it directly interferes with your blood’s ability to clot. Research shows it does this in three key ways: it slows down thrombin and factor Xa (two essential proteins in the clotting process), it extends the time it takes for blood to clot (measured as aPTT and PT), and it reduces platelet aggregation, meaning your blood cells stick together less easily.This isn’t theoretical. A 2012 study published in PubMed found curcumin’s anticoagulant effects were stronger than those of its derivative, bisdemethoxycurcumin. That means the very compound that makes turmeric yellow is also the one that can make your blood dangerously thin. And unlike prescription blood thinners, which are carefully calibrated, turmeric’s potency varies wildly. One capsule might have 50 mg of curcumin; another might have 500 mg. There’s no standard. That’s why doctors can’t predict how it will affect you.
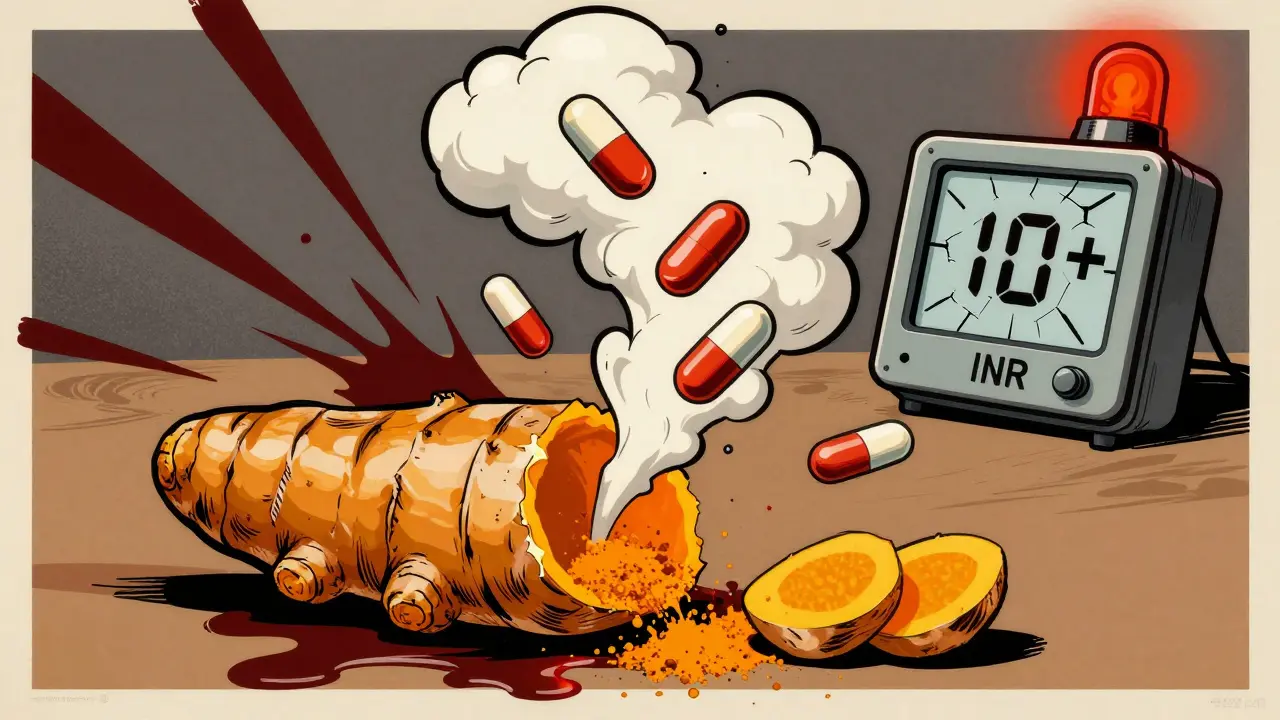
Real Cases of Dangerous Interactions
In April 2018, Medsafe in New Zealand issued a formal warning after a patient on stable warfarin therapy saw their INR - a measure of how long it takes blood to clot - jump from a normal 2.5 to over 10. That’s more than three times the upper limit of safety. INR above 10 means spontaneous bleeding can happen with little or no trauma. This patient wasn’t taking massive doses - just a daily turmeric supplement. They had no other changes in diet, medications, or health. The only new variable? Turmeric.Another case involved a kidney transplant patient who took 15 or more spoonfuls of turmeric powder daily for ten days. Their tacrolimus levels - a critical immunosuppressant - spiked to 29 ng/mL, far beyond the safe range. The result? Acute kidney injury. Turmeric didn’t just thin their blood - it disrupted how their body processed another life-saving drug. This isn’t an isolated incident. The Welsh Medicines Information Centre (WMIC) has documented multiple cases where turmeric caused unexpected spikes in drug levels, including norfloxacin and sulfasalazine, because it interferes with the CYP3A4 liver enzyme that breaks down many medications.
Which Blood Thinners Are Most at Risk?
Turmeric doesn’t just interact with one type of blood thinner - it risks interactions with nearly all of them:- Warfarin (Coumadin): The biggest concern. Warfarin has a narrow therapeutic window - the difference between working and causing bleeding is tiny. Turmeric can push INR levels into the danger zone quickly.
- DOACs (rivaroxaban, apixaban, dabigatran): Even newer drugs aren’t safe. The British Heart Foundation confirmed in 2023 that turmeric may interfere with these drugs, though the exact mechanism is still being studied.
- Aspirin, clopidogrel (Plavix): These are antiplatelet drugs, not anticoagulants, but turmeric also blocks platelet aggregation. Combining them doubles the anti-clotting effect.
- NSAIDs (ibuprofen, naproxen, diclofenac): These already raise bleeding risk. Add turmeric, and you’re stacking risks.
- Heparin, enoxaparin (Lovenox), dalteparin (Fragmin): Injectable anticoagulants used in hospitals and for deep vein thrombosis. Turmeric can amplify their effects unpredictably.
There’s no safe combination. Even if you’ve taken turmeric for years without issue, starting a supplement - or even increasing your curry intake - can trigger a reaction. The body doesn’t build tolerance to this effect. It just keeps building risk.
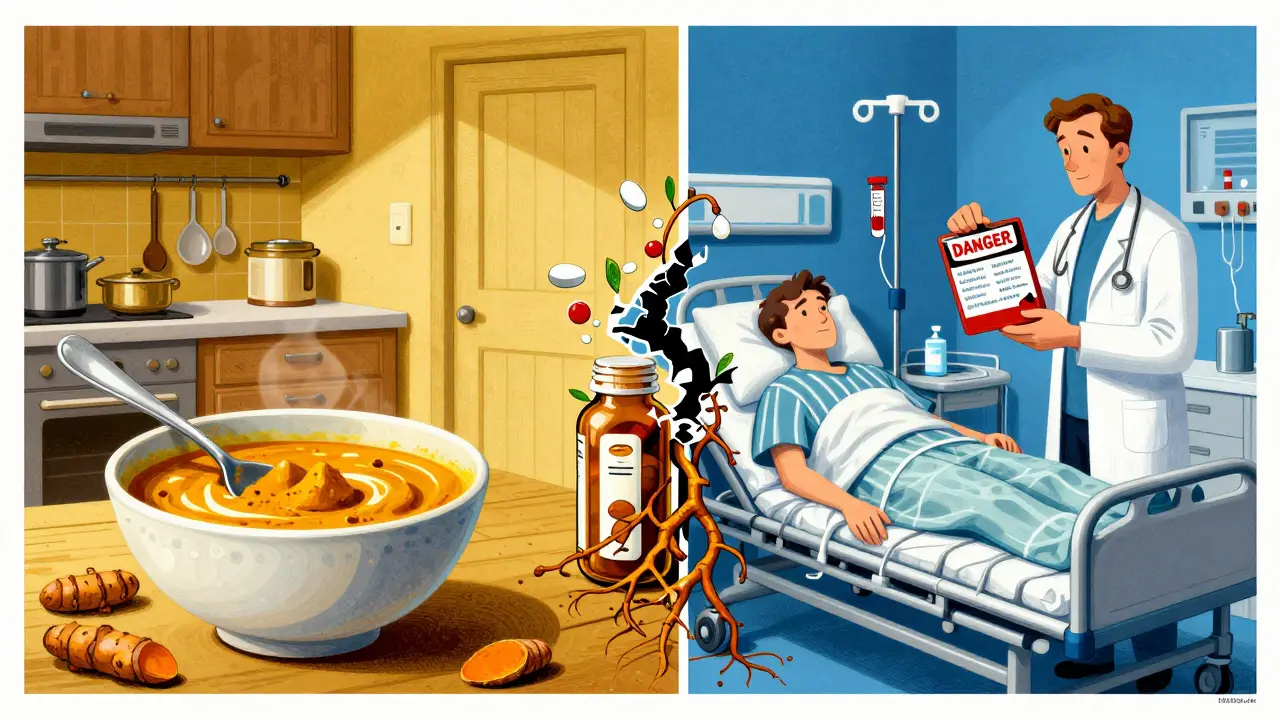
Why ‘Natural’ Doesn’t Mean Safe
People assume turmeric is harmless because it’s a spice. But that’s like saying aspirin is safe because it comes from willow bark. The dose makes the poison. Eating turmeric in food - a teaspoon in curry - is generally fine. But supplements? That’s a different story. A single capsule can contain the equivalent of 20 teaspoons of ground turmeric. And there’s no regulation on what’s actually inside most bottles.One 2023 analysis found that 30% of turmeric supplements on the market didn’t contain the labeled amount of curcumin. Some had none at all. Others had heavy metals or fillers. You can’t trust the label. And even if you could, the interaction risk isn’t linear. A small increase in curcumin intake can cause a disproportionate spike in anticoagulant effect, especially with warfarin.
Doctors don’t warn people about this because they assume patients will disclose supplement use. But most don’t. They think, “It’s just turmeric.” And by the time they realize something’s wrong - bruising easily, nosebleeds, blood in urine, a headache that won’t quit - it’s already an emergency.
What Doctors Say You Should Do
The message from Medsafe, WMIC, Mayo Clinic, and the British Heart Foundation is consistent:- Avoid turmeric supplements entirely if you’re on any blood thinner. Not “be careful.” Not “monitor.” Avoid.
- Don’t rely on “natural” labels. Supplements aren’t tested like drugs. No FDA approval. No clinical trials for interactions.
- Stop turmeric at least two weeks before any surgery - even dental work. Bleeding during procedures can be life-threatening.
- Inform every doctor and pharmacist about everything you take, including herbal products, teas, and smoothie powders.
- Stick to food amounts. Cooking with turmeric is unlikely to cause issues. But don’t add a spoonful to your morning smoothie thinking it’s a “health boost.”
The WMIC updated its guidance in October 2024, reinforcing that turmeric can reduce how quickly warfarin leaves the body - meaning it builds up, increasing bleeding risk over time. This isn’t a one-time effect. It’s cumulative. And because INR levels are checked only every few weeks for most patients, the danger can grow unnoticed.
What About Other Medications?
Turmeric doesn’t just play nice with blood thinners. It messes with a lot of other drugs too:- Tacrolimus: As seen in transplant patients, turmeric can spike levels, causing kidney damage.
- Sulfasalazine: One small study showed blood levels increased 3.2 times when taken with 2g of curcumin daily.
- Norfloxacin: Animal studies suggest turmeric increases its concentration, raising risk of side effects.
- Diabetes medications: Turmeric can lower blood sugar. Combined with insulin or metformin, that can lead to hypoglycemia.
If you’re on any chronic medication - for thyroid, heart, epilepsy, or mental health - turmeric might interfere. Always ask your pharmacist or doctor. Don’t assume it’s safe.
The Bottom Line
Turmeric isn’t evil. It’s not poison. But when you’re on a blood thinner, it becomes a hidden variable you can’t control. Prescription anticoagulants are designed with precise dosing, monitoring, and reversal agents. Turmeric isn’t. And that mismatch is deadly.If you’re taking warfarin, rivaroxaban, aspirin, or any other blood thinner, skip the turmeric capsules, pills, and powders. Don’t risk it. If you love the taste, keep using it in food - but don’t go beyond what you’d normally add to a meal. And if you’ve already started a supplement, stop. Talk to your doctor. Get an INR check. Your body doesn’t need the extra risk.
This isn’t about fear. It’s about facts. And the facts are clear: turmeric and blood thinners don’t mix safely. Not for you. Not for your family. Not even for someone who’s been healthy for years.
Can I take turmeric if I’m on warfarin?
No. Even small amounts of turmeric supplements can cause your INR to rise dangerously high - sometimes to levels over 10, which significantly increases your risk of uncontrolled bleeding. Medsafe and the Welsh Medicines Information Centre have issued formal warnings about this interaction. If you’re on warfarin, avoid turmeric supplements entirely.
Is cooking with turmeric safe while on blood thinners?
Yes, in normal food amounts. A teaspoon or two in curry, soup, or rice is unlikely to affect your blood clotting. The risk comes from concentrated supplements, powders, or extracts that deliver far more curcumin than you’d ever get from cooking. Stick to food - skip the pills.
What happens if I accidentally take turmeric with my blood thinner?
Stop taking the supplement immediately. Contact your doctor or pharmacist. If you notice unusual bruising, nosebleeds, blood in urine or stool, or a sudden headache, seek emergency care. Your INR may need to be checked right away. Don’t wait for symptoms - early detection saves lives.
Do all turmeric supplements have the same amount of curcumin?
No. Curcumin content varies widely - from 2% in raw turmeric to over 95% in some extracts. Many supplements don’t even contain what’s listed on the label. There’s no standardization, so you can’t predict how much curcumin you’re actually consuming. That’s why even “low-dose” supplements can be dangerous when combined with blood thinners.
How long should I stop turmeric before surgery?
The Mayo Clinic recommends stopping turmeric supplements at least two weeks before any surgery, including dental procedures. This gives your body time to clear the curcumin and reduces the risk of excessive bleeding during or after the procedure.
Are there any safe alternatives to turmeric for inflammation?
Yes. Omega-3 fatty acids from fish oil (in low doses) and ginger (in food amounts) have anti-inflammatory effects with less interaction risk. But even these should be discussed with your doctor if you’re on blood thinners. Never replace prescribed treatments with supplements without medical advice.