Every year, over 1.5 million people in the U.S. are harmed by medication errors. Many of these mistakes happen because patients don’t ask the right questions when picking up their prescriptions. The pharmacy counter isn’t just a place to get your pills - it’s your last line of defense against dangerous mistakes. Pharmacists are trained to catch errors, spot interactions, and explain what you’re really taking. But they can’t help if you don’t speak up.
What is this medication used for?
This seems obvious, but you’d be surprised how often people don’t know. You might get a new pill because your doctor said "it’ll help with your blood pressure," but never hear the actual name or purpose. If you can’t say it out loud - "I’m taking lisinopril to lower my blood pressure" - you’re at risk. Some medications have similar names. One person took a sleep aid thinking it was their heart medicine and ended up in the ER. Always confirm: What condition is this meant to treat? If the label says "for occasional pain," but your doctor said "for nerve pain," that’s a red flag.
How and when should I take this medication?
Dosage isn’t just about how many pills. It’s about timing, food, and even posture. Some pills must be taken on an empty stomach. Others need to be swallowed with a full glass of water. Some work better in the morning. Others should be taken at night. A 2023 study found that 41% of patients didn’t understand whether their medication should be taken with food or without. Take insulin, for example. If you store it wrong or take it after a meal instead of before, it can cause dangerous lows. Or consider antibiotics - if you skip doses or stop early because you feel better, you’re not just risking a return of the infection. You’re helping bacteria become resistant. Always ask: Do I take this with food? At the same time every day? Can I crush or split it?
What side effects should I expect - and which are dangerous?
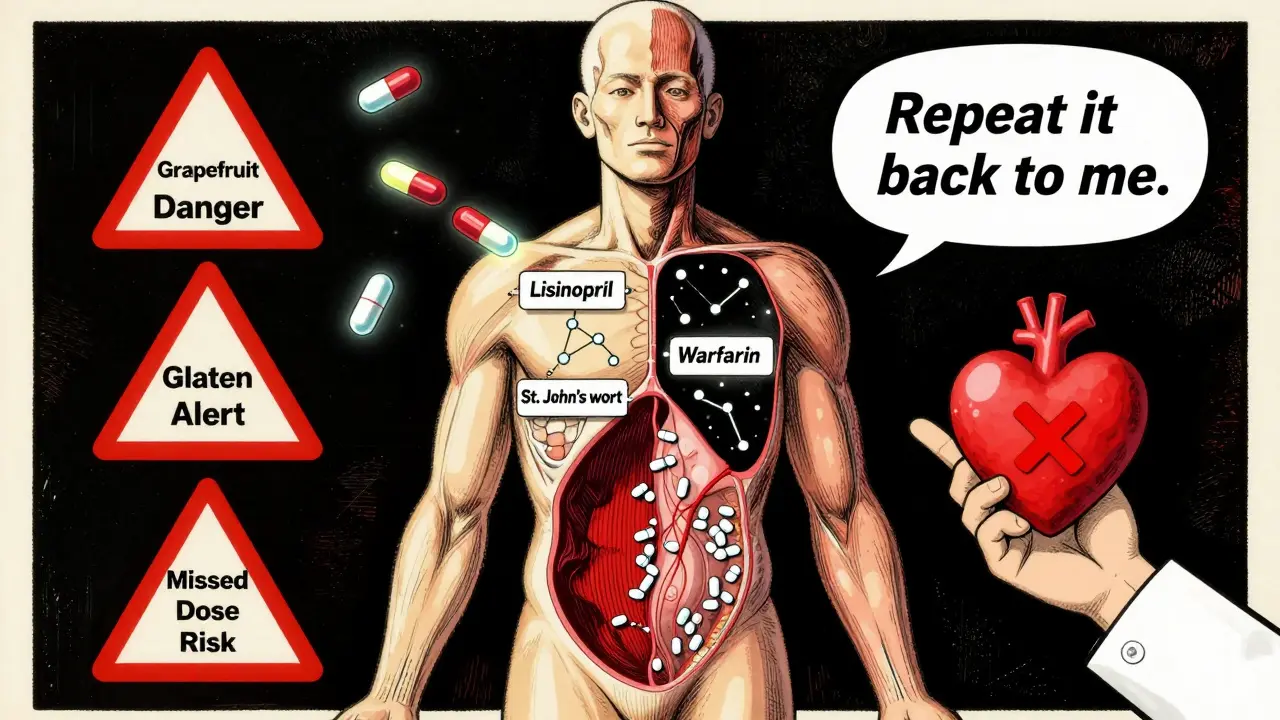
Not all side effects are emergencies. Some, like mild nausea or drowsiness, fade after a few days. Others mean trouble. The CDC reports that over 100,000 emergency room visits each year are due to unexpected drug reactions. Ask your pharmacist: What side effects are normal? Which ones mean I need to call a doctor right away? For example, if you’re on a blood thinner like warfarin, a headache or bruising might seem harmless. But if you start vomiting blood or have a sudden, severe headache, that could be internal bleeding. A 2022 FDA analysis showed that combining ibuprofen with blood thinners increases stomach bleeding risk by 40-60%. Don’t assume your pharmacist knows your full history. Tell them about every pill, supplement, and herbal tea you take.
Does this interact with my other meds, supplements, or food?
Most people think about prescription drugs only. But supplements, over-the-counter painkillers, and even grapefruit juice can cause serious problems. A 2023 survey by the American Pharmacists Association found that 89% of pharmacists caught a dangerous interaction during a patient consultation. One patient took St. John’s Wort for mood support while on an antidepressant - and ended up with serotonin syndrome, a life-threatening condition. Another took calcium supplements with thyroid medication and made both drugs useless. Even common items like antacids, vitamin D, or turmeric can interfere. Bring everything with you: pills, gummies, patches, eye drops, creams. Ask: Is there anything I should avoid eating, drinking, or taking with this? If you’re on blood pressure meds, for instance, salt substitutes can spike potassium levels dangerously. Grapefruit juice can make some cholesterol drugs toxic. These aren’t rare - they’re common.
Is there any ingredient that might cause an allergic reaction?
Allergies aren’t just about peanuts or shellfish. Some people react to dyes, fillers, or preservatives in pills. Red dye #40, lactose, or gluten can trigger rashes, swelling, or breathing trouble - even if you’ve never had a reaction before. Pocono Pharmacy’s 2023 guide notes that medication allergies cause over 106,000 ER visits each year. If you’ve ever had a rash from a pill, or swollen lips after taking something new, mention it. Ask: Does this contain any dyes, gluten, or lactose? If you’re on a low-sodium diet, check for sodium-based fillers. If you’re vegan, ask about gelatin capsules. These aren’t just "nice to know" - they’re critical.
How should I store this medication properly?
Heat, moisture, and light can turn medicine into junk - or worse. Insulin, for example, becomes useless if left in a hot car. Antibiotics can lose potency if not refrigerated. Some pills degrade if kept in the bathroom humidity. A pharmacist in Pennsylvania told Reddit users she’s seen insulin rendered useless because patients stored it in their glove compartments during summer. Others kept antibiotics in a drawer above the stove. Ask: Should this be refrigerated? Kept away from light? Stored in a dry place? If the bottle says "store below 77°F," don’t assume that means "room temperature." In a 90°F summer, "room temperature" is too hot. Also, never transfer pills to a different container unless it’s labeled. A woman once took her husband’s blood thinner thinking it was her aspirin - because both were in identical blue bottles.
Can I take this with my other health conditions?
Some medications are risky if you have kidney disease, liver problems, heart failure, or diabetes. A blood pressure pill might be fine for most people, but dangerous if your kidneys are weak. A painkiller might be okay for a healthy person but cause bleeding if you have ulcers. Your pharmacist doesn’t just see your list of drugs - they see your whole health picture. Ask: Is this safe with my other conditions? If you’re over 65, pregnant, or have chronic illness, this question alone can prevent hospitalization. The CDC says 35% of medication errors in kids under 12 happen because adults guess doses. But adults aren’t immune - 56% of hospital admissions involve medication mismatches because doctors didn’t know the patient’s full health history.
May I repeat back what you just told me?
This one’s powerful. A 2020 study in the Journal of the American Pharmacists Association found that when patients repeated instructions back, communication errors dropped by 31%. You don’t have to be perfect. Just say: "So, just to make sure I got this - I take one tablet every morning with water, avoid grapefruit, and call if I get a rash?" If the pharmacist says "Yes," you’re golden. If they correct you, you just avoided a mistake. This isn’t awkward - it’s smart. Pharmacists at Pocono Pharmacy started using this "teach-back" method in 2023 and saw a 44% drop in medication-related readmissions. If you’re nervous, bring someone with you. Or write it down. You’re not wasting their time - you’re making their job easier.
What if I miss a dose?
Life happens. You oversleep. You forget. You’re traveling. What do you do? Don’t guess. Don’t double up. Don’t skip it entirely. Ask: What should I do if I miss a dose? For some drugs, like birth control or blood pressure meds, missing one can cause a rebound effect. For others, like antibiotics, it can lead to resistance. A 2023 analysis by Johns Hopkins showed that patients who had clear instructions on missed doses were 29% less likely to have complications. Your pharmacist can give you a simple rule: "If you remember within 2 hours, take it. If it’s later, skip it and go back to your schedule." No more guessing.
Can I get a printed list of all my meds?
Most pharmacies can print a current list of everything you’re taking - including doses, times, and reasons. Keep it in your wallet. Bring it to every doctor visit. Update it every time something changes. The URMC Rochester Prescription Quiz found that 56% of hospital admissions involve medication discrepancies - meaning the patient’s list didn’t match what the doctor thought they were taking. That’s not a small mistake. That’s life-threatening. Ask for the list. Don’t wait for them to offer it. Say: Can you print me a current list of all my medications? It’s free. It’s fast. And it could save your life.
What if I want to stop taking this?
Some medications can’t be stopped cold. Antidepressants, blood pressure pills, seizure drugs - stopping suddenly can cause seizures, heart problems, or rebound symptoms. Even over-the-counter sleep aids can cause withdrawal. Ask: Is it safe to stop this? Do I need to taper off? One patient stopped her beta-blocker because she felt "fine" - and had a heart attack two weeks later. Don’t assume you’re okay just because you feel better. Your body might still need the drug. Always talk to your pharmacist before quitting anything.
What if I don’t understand what the pharmacist is saying?
Ask them to slow down. Say, "I’m not following - can you explain it again?" Or ask them to write it down. Many pharmacists have printed handouts or visual aids. You can also ask if they have a translator available. No question is too simple. Pharmacists are trained to help people who are confused - that’s part of their job.
Do I really need to bring all my pills to the pharmacy?
Yes. Bring everything - prescriptions, OTC painkillers, vitamins, herbal supplements, eye drops, creams, even patches. Many people forget these. But they all interact. A 2022 Johns Hopkins study showed that bringing all meds to a pharmacy review reduced dangerous drug combinations by 29%. Even if you think something is "harmless," like a fish oil capsule or a melatonin gummy, the pharmacist needs to know.
Can I ask about cheaper alternatives?
Absolutely. Pharmacists often know about generic versions, manufacturer coupons, or patient assistance programs. Some medications have multiple brands with the same active ingredient - one might cost $10, another $150. Ask: "Is there a less expensive option?" Many pharmacies offer $4 generic lists. Don’t assume you’re stuck with the price on the label.
What if I’m taking too many pills?
You’re not alone. Nearly half of adults over 65 take five or more medications. That’s called polypharmacy - and it increases risk of falls, confusion, and hospital stays. Ask your pharmacist: "Are all these still necessary?" They can review your list and flag duplicates, outdated prescriptions, or drugs that no longer match your condition. Some patients have cut their pill count by 30% after a simple review.
Can I get a refill reminder?
Most pharmacies offer text, email, or phone reminders. Ask for them. Missing refills leads to dangerous gaps - especially with heart, blood pressure, or mental health meds. A 2023 study found that patients who got refill reminders were 40% less likely to have a health crisis from missed doses. It’s a free service. Just ask.
Medication safety isn’t about being paranoid. It’s about being informed. You’re not just a patient - you’re a partner in your care. The pharmacist is there to help. But they can’t read your mind. If you walk away without asking questions, you’re leaving your safety to chance. Use these questions. Write them down. Bring them with you. Ask one at a time. Ask them all. Your life depends on it.
