What’s the Difference Between a TIA and a Stroke?
You wake up with sudden trouble speaking, your arm feels weak, and your vision blurs. Then, just as quickly as it started, it’s gone. You breathe a sigh of relief. TIA-you think it’s just a ‘mini-stroke.’ But here’s the truth: if you ignore it, you’re gambling with your life. A TIA isn’t a warning sign. It’s a full-blown stroke that didn’t stick. And it’s your body screaming for help.
The American Heart Association updated its definition in 2023: a TIA is a sudden loss of brain function caused by blocked blood flow, without permanent tissue damage. A stroke? That’s the same blockage-but now the brain tissue is dead. You can’t see the difference by symptoms alone. Both cause face drooping, arm weakness, slurred speech, vision loss, dizziness, or a sudden severe headache. The only real difference? One leaves scars. The other doesn’t. But that doesn’t mean the TIA is harmless.
Why a TIA Is More Dangerous Than It Looks
People think if symptoms disappear, the danger is over. That’s the deadliest myth in neurology. One in five people who have a TIA will have a full stroke within 90 days. And half of those strokes happen in the first two days. That’s not a coincidence. It’s a countdown.
Here’s what doctors now know: about 35% of people who come in with what looks like a TIA actually have a small stroke-just not one big enough to show up on a regular CT scan. Advanced MRI scans reveal tiny areas of dead brain tissue. These aren’t ‘minor’ events. They’re brain injuries that increase your risk of bigger ones. And the damage? It adds up. A 2022 study from the University of California found nearly half of people diagnosed with TIA had hidden brain damage detectable only with high-res imaging. This isn’t a false alarm. It’s a silent warning.
That’s why the old idea of waiting 24 hours to see if symptoms return is outdated-and dangerous. The clock starts ticking the moment symptoms begin. The longer you wait, the higher your chance of a stroke. The ABCD2 score-a simple tool doctors use-shows that if you’re over 60, have high blood pressure, weakness on one side, symptoms lasting more than a minute, and have diabetes? Your risk of stroke in 48 hours jumps to over 8%.
How to Spot a TIA or Stroke-Fast
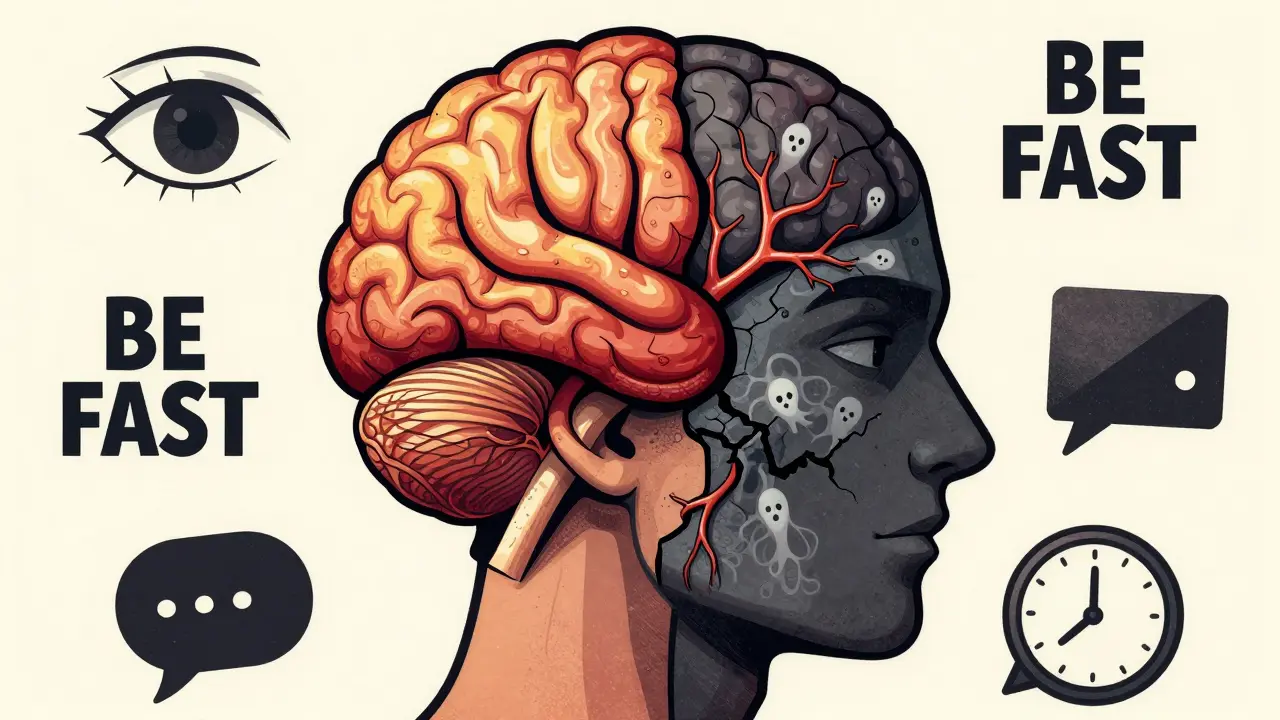
You don’t need to be a doctor to save a life. Use BE FAST:
- Balance: Sudden dizziness, loss of coordination, or trouble walking
- Eyes: Blurry, double, or lost vision in one or both eyes
- Face: One side droops when smiling. Ask them to smile. Is it uneven?
- Arm: One arm drifts down when raised. Ask them to lift both arms.
- Speech: Slurred, strange, or hard to understand. Ask them to repeat a simple sentence.
- Time: Call 911 now. Even if symptoms disappear.
It’s the same for TIA and stroke. No waiting. No hoping it’ll come back. If any of these happen, even briefly, call 911. Emergency responders don’t wait to diagnose. They get you to a hospital fast. And speed is everything.

What Happens in the ER
When you arrive, time is the most important factor. Hospitals have protocols. The first thing they do? Rule out bleeding in the brain with a non-contrast CT scan. That takes minutes. Then, they check your blood pressure, glucose, and heart rhythm. They’ll ask you the exact time symptoms started-down to the minute.
If you’re still having symptoms, they may give you clot-busting drugs like alteplase-but only if it’s been less than 4.5 hours since symptoms began. If symptoms are gone? They still treat you like you had a stroke. Because you might have.
Within 24 hours, you’ll get an MRI with diffusion-weighted imaging. This scan finds brain damage invisible to CT. If it shows a lesion? You didn’t have a TIA. You had a minor stroke. Either way, you’re now in high-risk territory.
Doctors use the ABCD2 score to decide if you need to be admitted. A score of 4 or higher? You’re going to the hospital overnight. Why? Because the risk of stroke is highest in the first 48 hours. And they need to start treatment immediately.
What Happens After the ER
Getting through the ER is just the first step. The real goal? Preventing the next stroke. And it’s not complicated.
- Aspirin: 325 mg within 24 hours cuts your next stroke risk by 60%.
- Dual antiplatelets: Aspirin + clopidogrel for 21 to 30 days reduces stroke risk by 80% in high-risk patients.
- High-intensity statin: Atorvastatin 80 mg daily lowers cholesterol and stabilizes artery plaques.
- Blood pressure control: Keep it under 140/90. Even lower if you have diabetes or kidney disease.
Some patients need surgery-like a carotid endarterectomy-if they have severe narrowing in the neck artery. Others need a heart monitor to catch silent atrial fibrillation, a common cause of clots.
And here’s the kicker: patients who get all this treatment within 48 hours cut their 90-day stroke risk from over 10% down to under 2%. That’s not a small difference. That’s life or death.
Why People Delay-And Why That’s Deadly
One in three people who have a TIA don’t seek help right away. Why? They think, ‘It’s gone, so it’s fine.’ Or, ‘I’ll call my doctor tomorrow.’
That’s a mistake. CDC data shows 31% of TIA patients wait more than 24 hours. By then, the window for prevention is closing. And the damage? It’s already happening.
There’s also confusion around terminology. Calling it a ‘mini-stroke’ makes people think it’s not serious. It’s not. It’s a full stroke that didn’t stick. And the brain doesn’t care how long the blockage lasted. What matters is whether tissue died. And often, it did.
Programs like SOS-TIA at Massachusetts General Hospital show what works: same-day evaluation for every TIA patient. They cut 90-day stroke risk to just 1.2%. Compare that to the 10.3% risk when people wait. That’s an 88% reduction. All because someone called 911 instead of waiting.
What’s Changing in TIA Care
The rules are evolving. The Joint Commission now requires stroke centers to have dedicated TIA pathways. Hospitals that don’t evaluate high-risk TIA patients within 24 hours risk losing certification-and funding.
Telemedicine clinics are popping up. You can get a neurologist consult within hours, even from home. AI tools now predict stroke risk with over 90% accuracy by combining imaging, blood tests, and symptoms.
And soon? A simple blood test might tell you within 15 minutes if you had a brain injury. Glial fibrillary acidic protein (GFAP) is being tested right now. If it works, we won’t need MRI to know if damage occurred. We’ll know in minutes.
Medicare now penalizes hospitals with more than 20% of TIA patients having a stroke within 30 days. That’s driving hospitals to act fast. And it’s saving lives.
What You Need to Do Right Now
If you or someone you know had sudden symptoms-even if they’re gone-call 911. Don’t wait. Don’t call your doctor. Don’t ‘see how it feels tomorrow.’
If you’ve had a TIA before, make sure you’re on aspirin or clopidogrel. Take your statin. Control your blood pressure. Get your heart checked. Don’t skip follow-ups. The risk doesn’t disappear after 90 days. It just changes.
And if you’re over 50, with high blood pressure, diabetes, or a history of smoking? Talk to your doctor about a TIA risk assessment. You don’t need to wait for symptoms to strike.
Every minute counts. Every second matters. A TIA isn’t a scare. It’s a signal. And if you ignore it, you’re not just risking a stroke. You’re risking your life.
Frequently Asked Questions
Can a TIA cause permanent damage?
Traditionally, yes-TIA was defined by the absence of permanent damage. But modern imaging shows that up to 48% of people diagnosed with TIA have tiny areas of brain injury that aren’t visible on standard scans. These changes may not cause obvious symptoms, but they increase your risk of future strokes and cognitive decline. So even if you feel fine, there may be hidden damage.
Is a TIA the same as a mini-stroke?
No. The term ‘mini-stroke’ is misleading and dangerous. It suggests the event is minor or harmless. But a TIA is a full stroke event-just one that didn’t leave lasting damage. The brain experienced the same blockage. The difference is whether tissue died. Calling it a ‘mini-stroke’ leads people to ignore symptoms, which increases their risk of a real stroke. Doctors now avoid this term entirely.
How long do TIA symptoms last?
Most TIA symptoms resolve within 10 to 60 minutes, with over half gone in under 30 minutes. But duration doesn’t determine severity. Even if symptoms last only 5 minutes, if they’re caused by a blocked artery, you’re at high risk for a stroke. The new medical definition no longer uses time as a criterion-only whether brain tissue shows damage on MRI.
Do I need imaging after a TIA?
Yes. A CT scan is done first to rule out bleeding. But it can’t detect small areas of brain injury. An MRI with diffusion-weighted imaging is the gold standard-it finds 99% of acute strokes, even tiny ones. If you had a TIA, you need this scan within 24 hours. It’s not optional. It changes your treatment plan.
Can I prevent a stroke after a TIA?
Absolutely. If you get treated within 48 hours, your risk of stroke drops by 80%. That means taking aspirin or dual antiplatelets, starting a high-dose statin, controlling blood pressure, and checking for heart rhythm problems like atrial fibrillation. Lifestyle changes-quitting smoking, eating better, moving more-also help. But medication is the most powerful tool in the first critical days.
Should I call 911 if symptoms go away?
Yes. Always. Emergency responders can start treatment en route. They know how to prioritize you. Hospitals have special TIA pathways that get you seen within an hour. If you drive yourself or wait, you risk missing the critical window. Symptoms disappearing doesn’t mean the danger is gone. It means you’re in the highest-risk period.
Who is most at risk for a TIA?
People over 60, especially those with high blood pressure, diabetes, smoking history, obesity, or atrial fibrillation. Men are slightly more likely than women to have a TIA, but women have higher long-term stroke risk after a TIA. Black and Hispanic populations also face higher rates due to higher rates of hypertension and diabetes. Age is the biggest factor-the median age for TIA is 69.