Insulin Resistance Explained: Impact on Cholesterol and Simple Fixes
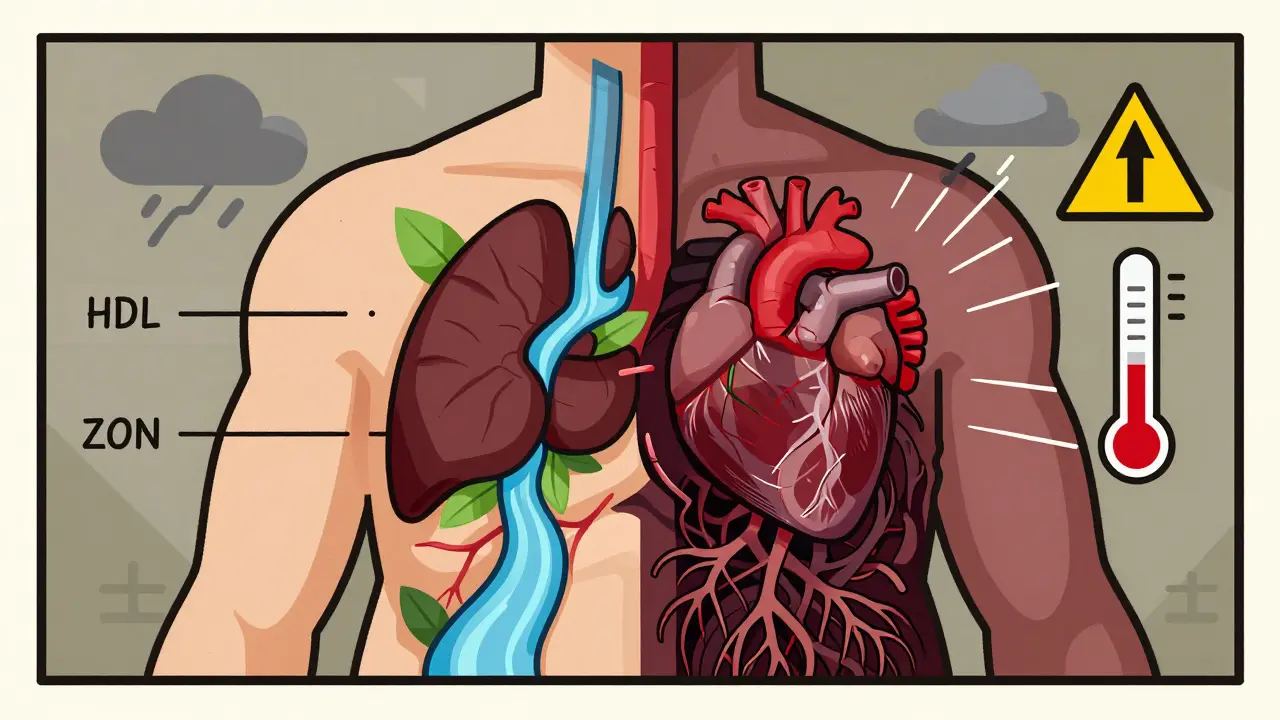
Ever wonder why your cholesterol numbers spike even when you eat a low‑fat diet? The hidden culprit is often insulin resistance. When your cells stop responding properly to insulin, your liver makes more bad cholesterol (LDL) and fewer good particles (HDL). The result? A higher risk of heart disease, even if you think you’re doing everything right.
Insulin resistance doesn’t just affect blood sugar; it messes with the whole metabolic system. Your body stores excess glucose as fat, especially around the belly, and that fat releases inflammatory chemicals. Those chemicals tell the liver to crank up production of triglycerides and lower HDL. So, the more resistant you are, the worse your cholesterol profile becomes.
How Insulin Resistance Affects Your Cholesterol Levels
First, insulin normally tells the liver to pull cholesterol out of the bloodstream. When resistance builds, the signal weakens, and the liver lets more LDL float around. Second, high insulin levels push the liver to create tiny, dense LDL particles, which are more likely to stick to artery walls. Third, insulin resistance raises triglycerides because the body can’t clear them efficiently. High triglycerides often coincide with low HDL, the protective cholesterol that helps remove plaque.
All three changes—more LDL, more triglycerides, and less HDL—create a perfect storm for atherosclerosis. That’s why doctors look at the “metabolic syndrome” cluster: waist size, blood pressure, fasting glucose, triglycerides, and HDL. Spotting insulin resistance early can stop the cholesterol climb before it becomes a heart‑attack risk.
Practical Steps to Improve Insulin Sensitivity
Good news: you can tweak everyday habits to boost insulin sensitivity and tame cholesterol. Start with your plate: swap refined carbs and sugary drinks for high‑fiber foods like oats, beans, and non‑starchy veggies. Fiber slows glucose absorption, keeping insulin spikes low.
Next, add a dose of healthy fats—think olive oil, nuts, and avocado. These fats don’t trigger insulin spikes and actually help raise HDL. Pair them with a modest amount of protein at each meal to keep blood sugar steady.
Exercise is a powerhouse move. Just 30 minutes of brisk walking, cycling, or strength training a few times a week can make muscles take up glucose without needing extra insulin. Consistency beats intensity; even short, frequent walks beat a single marathon session for insulin benefit.
Sleep and stress matter, too. Aim for 7‑8 hours of quality sleep and practice stress‑relief techniques like deep breathing or meditation. Poor sleep raises cortisol, which worsens insulin resistance, while chronic stress does the same.
Finally, consider a quick health check. A simple fasting insulin or HOMA‑IR test can tell you how resistant you are. If numbers are high, talk to a clinician about possible supplements like magnesium or vitamin D, which some studies link to better insulin action.
Bottom line: insulin resistance is a silent driver of bad cholesterol. By adjusting diet, moving more, and managing sleep and stress, you can flip the switch on insulin sensitivity, lower LDL, raise HDL, and protect your heart without pricey meds.
Metabolic Syndrome: The Cluster of Heart Disease Risk Factors You Can't Ignore
Metabolic syndrome is a dangerous cluster of heart disease risk factors including belly fat, high blood pressure, and abnormal cholesterol. It affects 1 in 3 U.S. adults and can be reversed with lifestyle changes.
Learn more...Secondary Hypogonadism and Type 2 Diabetes: Causes, Diagnosis, and Treatment Guide
Up to one-third of men with type 2 diabetes have reversible low testosterone. Learn the causes, tests, and safe treatment options that actually move the needle.
Learn more...