Sulfonamide Cross-Reactivity Checker
Check if Your Medication is Safe
This tool helps determine if a sulfonamide-containing medication is safe to take based on your documented sulfa allergy. It's based on scientific evidence about cross-reactivity between different types of sulfonamides.
Many people carry a label in their medical record: sulfa allergy. It sounds simple. But what it actually means - and what you should avoid - is far more complicated than most doctors and patients realize.
Chances are, if you’ve been told you’re allergic to sulfa, you’ve been given the wrong advice. You might have avoided blood pressure meds, diuretics, or even pain relievers for years - not because you had a real reaction, but because someone misread a vague note from decades ago. The truth? Most people with a documented sulfa allergy aren’t allergic at all. And even if you are, you likely can still safely take many common medications that contain sulfur.
What Is a True Sulfa Allergy?
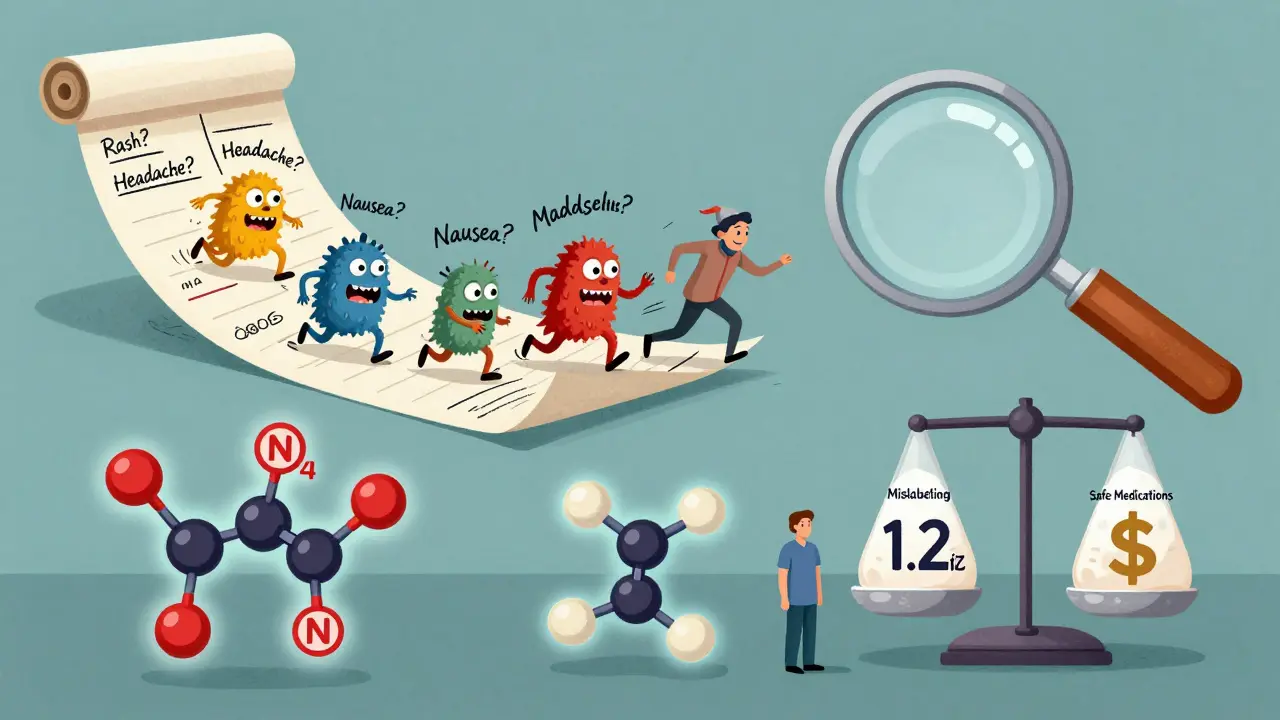
A true sulfonamide antibiotic allergy is rare. Only about 0.3% to 0.5% of the population has a real IgE-mediated reaction to drugs like sulfamethoxazole or sulfadiazine. Yet, 3% to 12% of people claim a sulfa allergy in their charts. That’s a huge gap. Why?
Because most reactions aren’t allergies at all. A rash that shows up a week after taking an antibiotic? That’s often just a side effect - not an immune response. Nausea, headache, dizziness? Those are common drug reactions, not allergies. Even a mild skin rash after taking sulfamethoxazole-trimethoprim (Bactrim) doesn’t automatically mean you’re allergic. Many people are labeled as allergic based on vague symptoms that don’t meet the clinical definition of an allergic reaction.
True allergic reactions to sulfonamide antibiotics happen quickly - within minutes to hours - and involve symptoms like hives, swelling, trouble breathing, or anaphylaxis. Or, in rare but serious cases, they cause life-threatening skin conditions like Stevens-Johnson syndrome or toxic epidermal necrolysis. These are the only reactions that matter when considering future drug use.
The Big Misconception: All Sulfonamides Are the Same
Here’s where things get confusing - and dangerous. The word "sulfa" gets thrown around like it’s one thing. But there are two very different kinds of sulfonamides: antimicrobial and nonantimicrobial.
Antimicrobial sulfonamides - the ones you take as antibiotics - have a very specific chemical structure. They contain an arylamine group at the N4 position and a nitrogen-containing ring at the N1 position. These parts are what make them effective against bacteria - and what can trigger an immune response in rare cases.
Nonantimicrobial sulfonamides? They look different. They don’t have those exact chemical features. That’s why drugs like hydrochlorothiazide (for high blood pressure), furosemide (a water pill), celecoxib (Celebrex), and acetazolamide (for glaucoma or altitude sickness) are not cross-reactive with antibiotic sulfonamides.
Think of it this way: All squares are rectangles, but not all rectangles are squares. All antimicrobial sulfonamides are sulfonamides, but not all sulfonamides are antimicrobial. The chemistry is different. The risk is different.
What You Can Still Take - Even With a Sulfa Allergy
If you’ve been told to avoid all "sulfa" drugs, here’s what you’re probably being wrongly denied:
- Hydrochlorothiazide - A first-line treatment for high blood pressure. Studies show the reaction risk in people with sulfonamide antibiotic allergy is only 1.1%, compared to 0.9% in people with no allergy. That’s not a risk - it’s noise.
- Furosemide - Used for heart failure and fluid retention. No proven cross-reactivity.
- Celecoxib - A COX-2 inhibitor for arthritis pain. Over 10,000 patients studied showed no increased risk of reaction.
- Acetazolamide - Used for glaucoma, epilepsy, and altitude sickness. Safe in nearly all cases.
- Sumatriptan - For migraines. Contains a sulfonamide group but lacks the allergenic structure.
These medications are not just safe - they’re often the best, safest, or cheapest option. Yet, patients with a "sulfa allergy" label are 2.4 times more likely to get a fluoroquinolone like ciprofloxacin instead - a drug with black box warnings for tendon rupture and aortic aneurysm.
The One Exception: Dapsone
There’s one nonantimicrobial sulfonamide that does carry a higher risk: dapsone. It’s used to prevent Pneumocystis pneumonia in people with HIV or autoimmune conditions. Dapsone shares enough structural similarity with antibiotic sulfonamides that some patients with a true sulfa allergy may react to it. Studies show a reaction rate of about 13% in those with prior sulfonamide antibiotic allergies.
If you’ve had a severe reaction to a sulfonamide antibiotic - like a blistering rash or anaphylaxis - your doctor should proceed with caution with dapsone. But even then, many patients can tolerate it under supervision. A 2022 study found that 91.5% of patients with "sulfa allergy" who were given dapsone under medical supervision had no reaction.
What About Sulfates, Sulfites, and Sulfur?
Let’s clear up another big myth: sulfonamide allergy has nothing to do with sulfur, sulfates, or sulfites.
Sulfur is an element. Sulfates (like magnesium sulfate) are salts used in Epsom baths or to treat eclampsia. Sulfites are preservatives in wine and dried fruit. None of these contain the sulfonamide group. None of them trigger the same immune response.
Yet, a 2020 survey found that nearly 43% of primary care doctors thought patients with sulfa allergies couldn’t take sulfites. That’s wrong. And it’s dangerous. Patients with asthma who avoid sulfites because of a "sulfa allergy" are missing out on critical treatments - or being told they can’t eat dried fruit or drink wine unnecessarily.
Why This Matters: The Real Cost of Mislabeling
This isn’t just about convenience. It’s about survival.
When doctors avoid sulfonamide antibiotics because of a mislabeled allergy, they turn to broader-spectrum drugs like vancomycin, clindamycin, or fluoroquinolones. These are more expensive, more toxic, and more likely to cause antibiotic resistance. A 2021 study showed that patients with a "sulfa allergy" label received broader antibiotics 32.7% of the time - even when sulfonamides were the best choice.
The financial toll? Over $1.2 billion a year in the U.S. alone. That’s extra hospital stays, longer treatments, and more resistant infections. The CDC links this mislabeling to an 8.3% increase in E. coli resistance and a 12.7% rise in Staphylococcus aureus resistance.
And for patients? It means being denied the right treatment for years. One patient, a 68-year-old man, avoided hydrochlorothiazide for 15 years because of a childhood rash. He ended up with poorly controlled blood pressure and more side effects from other meds. When he finally saw an allergist, he passed a simple oral challenge - and was put on the right drug.
What Should You Do?
If you’ve been told you have a sulfa allergy, here’s what to do next:
- Look at your medical record. What was the actual reaction? "Rash" isn’t enough. Was it immediate? Did you have trouble breathing? Was it a blistering rash? Write it down.
- Ask your doctor: "Was this a true allergic reaction, or just a side effect?" If it was a mild rash that showed up after five days, it’s likely not an allergy.
- Consider an allergy evaluation. If you’ve avoided important meds for years, ask for a referral to an allergist. They can do a skin test or oral challenge - both are safe and highly accurate.
- Update your records. If you’re cleared, make sure your doctor changes "sulfa allergy" to "no true allergy" or "tolerated sulfonamide antibiotics." This helps every future provider.
Don’t let an outdated label control your care. You don’t need to avoid hydrochlorothiazide, celecoxib, or furosemide because of a childhood rash. You don’t need to fear sulfates or sulfites. And you don’t need to take riskier, more expensive drugs just because someone wrote "sulfa allergy" on a chart 20 years ago.
What About Future Testing?
There’s promising research on the horizon. A new blood test for sulfamethoxazole-specific IgE is in Phase II trials and shows 89.7% accuracy in predicting true allergies. By 2025, most major health systems are expected to use automated tools in their electronic records that flag whether a reaction was likely real - and suggest safer alternatives.
But you don’t have to wait. The tools are already here: your medical history, your doctor’s questions, and a simple oral challenge under supervision. You don’t need fancy tech to find out if you’re truly allergic. You just need the right information.
Stop avoiding what you don’t need to avoid. Start asking the right questions. Your health - and your future prescriptions - depend on it.
Can I take hydrochlorothiazide if I have a sulfa allergy?
Yes, you can. Hydrochlorothiazide is a nonantimicrobial sulfonamide and does not share the chemical structure that causes allergic reactions to antibiotic sulfonamides. Studies show the risk of reaction is only about 1.1% - the same as in people with no sulfa allergy. Most patients with a history of sulfonamide antibiotic allergy tolerate hydrochlorothiazide without issue.
Is celecoxib safe for people with sulfa allergies?
Yes. Celecoxib (Celebrex) is a nonantimicrobial sulfonamide. It lacks the arylamine group that triggers allergic reactions in antibiotic sulfonamides. A large 2021 study of over 10,000 patients found no increased risk of reaction in those with sulfonamide antibiotic allergies. It is considered safe for use in this population.
Do sulfonamide allergies mean I can’t take sulfur or sulfites?
No. Sulfur, sulfates (like magnesium sulfate), and sulfites (used in wine and dried fruit) are chemically unrelated to sulfonamide drugs. A sulfonamide allergy does not mean you’re allergic to these substances. This is a common misconception - even among some doctors - but it’s not based on science.
What’s the difference between antimicrobial and nonantimicrobial sulfonamides?
Antimicrobial sulfonamides (like sulfamethoxazole) have a specific chemical structure: an arylamine group at the N4 position and a nitrogen-containing ring at the N1 position. These parts are what make them effective antibiotics - and what can trigger allergies. Nonantimicrobial sulfonamides (like hydrochlorothiazide or celecoxib) lack these groups. Their chemistry is different, and they don’t cause cross-reactivity.
Should I get tested if I think I have a sulfa allergy?
If you’ve avoided important medications because of a vague "sulfa allergy" label, yes. If your reaction was mild (like a rash that appeared days after starting the drug), you’re likely not allergic. An allergist can perform a skin test or oral challenge to confirm. Over 90% of people labeled with sulfa allergy pass these tests and can safely take sulfonamide antibiotics or nonantimicrobial sulfonamides.
Can a sulfa allergy label cause antibiotic resistance?
Yes. When doctors avoid sulfonamide antibiotics because of a mislabeled allergy, they often prescribe broader-spectrum drugs like fluoroquinolones or vancomycin. These drugs are more likely to promote antibiotic-resistant bacteria. Studies show this practice increases resistance rates in common infections like E. coli and Staphylococcus aureus by up to 13%.