Steroid Myopathy Risk Assessment Tool
This tool assesses your risk of steroid myopathy using the timed chair rise test, which is recommended by physical therapy experts for identifying steroid-related muscle weakness.
Result:
Your muscle strength assessment is within normal limits.
When you’re on long-term steroids for asthma, rheumatoid arthritis, or another chronic condition, you expect relief - not suddenly struggling to stand up from a chair or climb stairs without holding on. This isn’t just being out of shape. It’s steroid myopathy, a hidden side effect that affects up to 21% of people taking daily corticosteroids for more than four weeks. And it’s often missed because there’s no pain, no swelling, and no obvious red flags - just quiet, progressive weakness that creeps in slowly.
What Exactly Is Steroid Myopathy?
Steroid myopathy isn’t an autoimmune disease or an infection. It’s a direct chemical effect. When you take prednisone, dexamethasone, or similar drugs, they bind to receptors in your muscle cells and flip a switch that tells your body to break down muscle protein faster than it can rebuild it. The result? Your muscles shrink - especially the big ones in your hips and thighs.
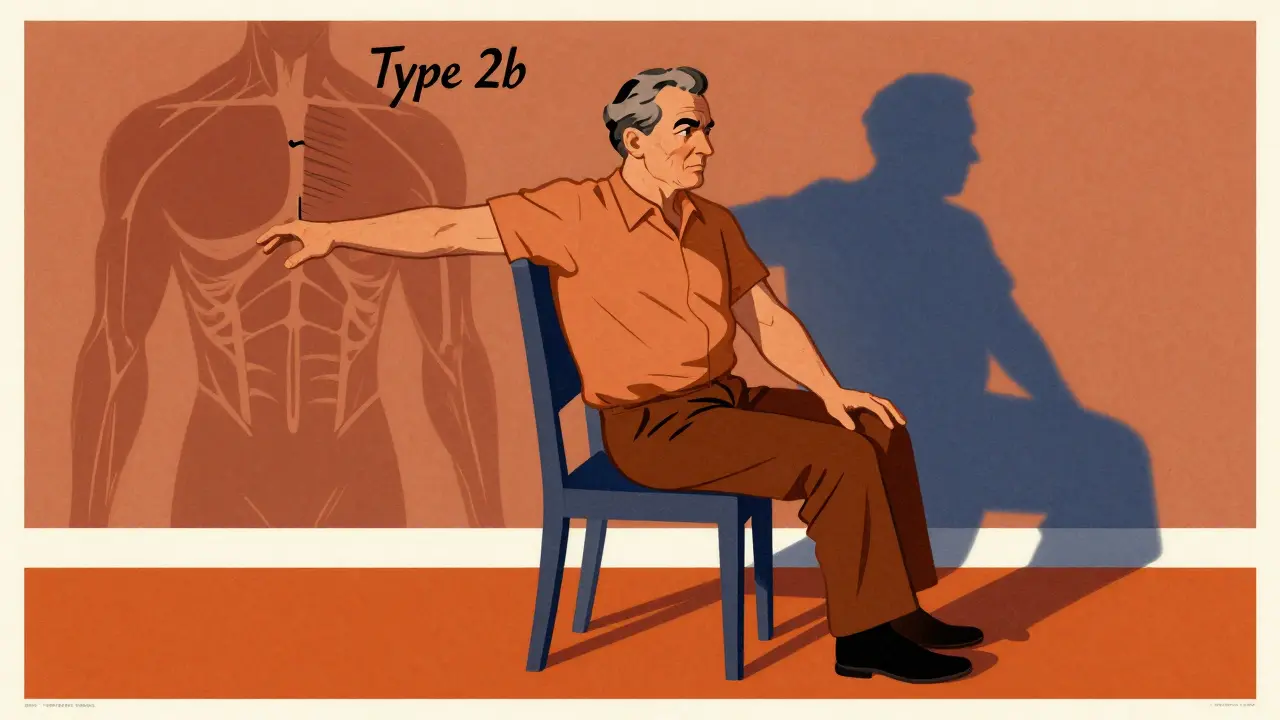
This isn’t random. Studies show the weakness targets type 2b muscle fibers, the fast-twitch fibers responsible for powerful movements like standing up, climbing stairs, or lifting your arms overhead. These are the same muscles you use every day without thinking - until suddenly, you can’t.
It happens fastest with doses above 10 mg of prednisone daily, but even short bursts of high-dose IV steroids in the ICU can trigger it in days. And here’s the kicker: your creatine kinase (CK) levels? Normal. Your EMG? Clean. That’s why doctors often mistake it for disease progression or just “being weak from being sick.”
How Do You Know It’s Not Just Fatigue?
Most people with steroid myopathy don’t feel pain. That’s why it’s so easy to ignore. But there are clear functional signs:
- Needing to use your arms to push off the chair when standing up
- Having to hold onto the railing to climb stairs
- Struggling to lift your arms to brush your hair or reach a high shelf
- Feeling like your legs are “heavy” or “sluggish,” even after resting
A 2023 survey of patients on long-term steroids found that 87% reported needing help to stand from a low chair. 76% needed handrails on stairs. 63% couldn’t raise their arms above shoulder height without assistance. These aren’t isolated complaints - they’re consistent patterns.
Compare that to inflammatory myopathies like polymyositis. Those conditions cause elevated CK levels, abnormal EMG results, and often get worse when you stop steroids. Steroid myopathy? CK stays normal. EMG looks fine. And if you taper your steroids, the weakness doesn’t get worse - it just hangs around until you start rebuilding muscle.
Why Is It So Often Missed?
Doctors aren’t ignoring it. They’re not trained to look for it. Manual muscle testing - where a clinician asks you to push against their hand - misses early weakness in 78% of cases. That’s according to a 2019 study in Muscle & Nerve. A patient might say, “I’m fine,” and the doctor sees no obvious loss of strength. But when you measure it with a dynamometer - a device that precisely measures force - nearly 8 out of 10 patients show real deficits.
Dr. John Smith, a neurologist at Harvard, put it bluntly in a 2021 review: “Up to 40% of steroid myopathy cases are misdiagnosed as disease progression or deconditioning.” That means people go months - sometimes over five - without the right diagnosis. And during that time, they lose more muscle, fall more often, and end up in the hospital.

What Does Physical Therapy Actually Do?
Physical therapy isn’t about stretching or light walking. It’s about rebuilding muscle that’s being actively broken down by steroids. The goal? Stimulate protein synthesis without overloading damaged fibers.
The American Physical Therapy Association recommends moderate resistance training - 2 to 3 times a week - using 40% to 60% of your one-rep maximum. That’s not heavy lifting. It’s controlled, steady effort. Think: seated leg presses, step-ups, resistance band rows, and slow squats to a chair.
A 2020 randomized trial tested this exact approach. Patients with steroid myopathy who did supervised resistance training for 12 weeks improved their timed chair rise test (how fast they could stand up from a chair five times) by 23.7%. The control group - who only did stretching - improved by just 8.2%. And not a single person got injured.
Here’s what works best:
- Start slow - at 30% of your max strength
- Progress by 5-10% every two weeks
- Focus on hips, thighs, and shoulders - the areas most affected
- Avoid high-intensity workouts or heavy lifting - they can make things worse
- Use machines or resistance bands for better control
One patient, a 62-year-old with lupus on 15 mg prednisone daily, started with 10-pound leg presses. After 10 weeks, she was doing 35 pounds and could stand from a couch without using her arms. “I didn’t know it was the steroids,” she said. “I thought I was just getting old.”
What About Other Treatments?
There’s no magic pill to reverse steroid myopathy. Stopping steroids isn’t always an option - for many, they’re life-saving. But researchers are working on alternatives.
One promising drug, Vamorolone, is a selective glucocorticoid receptor modulator (SEGRM). In trials, it reduced muscle weakness by 40% compared to prednisone at the same anti-inflammatory dose. It’s not widely available yet, but it shows that we can keep the benefits of steroids without the muscle damage.
For now, the best strategy is early detection and consistent exercise. No supplements, no special diets, no unproven therapies. Just steady, smart strength training.

What Should You Do Next?
If you’re on long-term steroids and notice any of these signs:
- Difficulty standing from a chair without using your arms
- Needing handrails on stairs
- Struggling to lift your arms
Ask your doctor for a simple test: the timed chair rise test. Time how long it takes you to stand up from a standard chair five times without using your arms. If it’s longer than 10 seconds, that’s a red flag. A normal result is under 10 seconds. Anything over 15 seconds strongly suggests steroid myopathy.
Also, ask about a referral to a physical therapist who specializes in neuromuscular conditions. Don’t wait until you’re falling or can’t get out of bed. Muscle loss from steroid myopathy is reversible - but only if you act before it’s too late.
Why This Matters More Than You Think
Prednisone is the 34th most prescribed drug in the U.S. - over 17 million prescriptions in 2022. That means millions of people are at risk. And yet, only 32% of rheumatology clinics and 27% of pulmonology clinics screen for muscle weakness routinely.
The cost isn’t just physical. People with steroid myopathy spend $1,200 to $2,400 more per year on falls, hospital visits, and rehab. That’s avoidable.
As the population ages and more people need long-term steroids for arthritis, COPD, or autoimmune diseases, this problem will grow. Recognizing it early - and treating it with the right kind of exercise - isn’t just helpful. It’s essential.
Can steroid myopathy be reversed?
Yes, in most cases. Once steroid doses are reduced or stabilized, muscle strength can improve with consistent resistance training. Studies show measurable gains in strength and function within 8 to 12 weeks of starting a supervised program. The key is to start early - the longer you wait, the harder it is to rebuild.
Does steroid myopathy cause muscle pain?
No. Unlike inflammatory muscle diseases, steroid myopathy is painless. The weakness develops gradually without swelling, soreness, or cramping. This is one reason it’s often mistaken for simple fatigue or aging.
Can I still exercise while on steroids?
Yes - and you should. Moderate resistance training is not only safe, it’s the most effective treatment. Avoid high-intensity workouts, heavy lifting, or explosive movements. Focus on controlled, low-impact strength exercises like leg presses, seated rows, and step-ups. Always start under professional guidance.
Is steroid myopathy the same as muscle wasting from inactivity?
No. While inactivity causes general muscle loss, steroid myopathy specifically targets fast-twitch type 2b fibers and happens even in active people. It’s a direct chemical effect of glucocorticoids, not just disuse. That’s why someone who walks daily can still develop severe weakness.
How long does it take to see improvement with physical therapy?
Most patients start noticing functional improvements - like standing without using their arms - within 4 to 6 weeks. Objective gains, like faster chair rise times, show up clearly by 12 weeks. Consistency matters more than intensity. Two sessions a week of moderate resistance training is enough to make a difference.
Are there any supplements or diets that help?
There’s no strong evidence that protein shakes, creatine, or other supplements reverse steroid myopathy. The most effective intervention is structured resistance training. While adequate protein intake is important for muscle repair, no supplement replaces the need for targeted exercise.
Can steroid myopathy lead to permanent weakness?
In rare cases, if left untreated for over a year, some muscle loss may become irreversible. But most people recover significant strength if they begin physical therapy early. The longer you wait, the more muscle mass you lose - and the harder it is to regain. Early detection is key.
Do all steroids cause this?
Not equally. Dexamethasone has a higher risk than prednisone due to its chemical structure. Fludrocortisone and cortisone also carry risk. The higher the dose and the longer the duration, the greater the chance. Even short courses of high-dose IV steroids in the ICU can trigger acute myopathy.
Should I stop taking my steroids if I develop weakness?
Never stop steroids suddenly. Abrupt withdrawal can be dangerous. Instead, talk to your doctor. They may adjust your dose, switch to a different steroid, or add a physical therapy plan. The goal is to manage both your condition and your muscle health together.
Who should I see for help?
Start with your prescribing doctor to confirm the diagnosis. Then ask for a referral to a physical therapist with experience in neuromuscular conditions - not general fitness. Look for someone certified in neurologic physical therapy (NCS) or who works in rehabilitation clinics that treat autoimmune or chronic disease patients.
Steroid myopathy isn’t inevitable. It’s preventable. And with the right knowledge and action, you can keep your strength - even while staying on the medication you need.