When you start taking an SGLT2 inhibitor like Jardiance, Farxiga, or Invokana for type 2 diabetes, you might not expect to feel dizzy or unusually thirsty. But these side effects aren’t rare - they’re built into how the drug works. SGLT2 inhibitors don’t just lower blood sugar. They act like mild diuretics, pulling extra water and salt out of your body through urine. That’s why many people lose a few pounds in the first week - not from dieting, but from fluid loss. And that fluid loss is what leads to dehydration, dizziness, and drops in blood pressure.
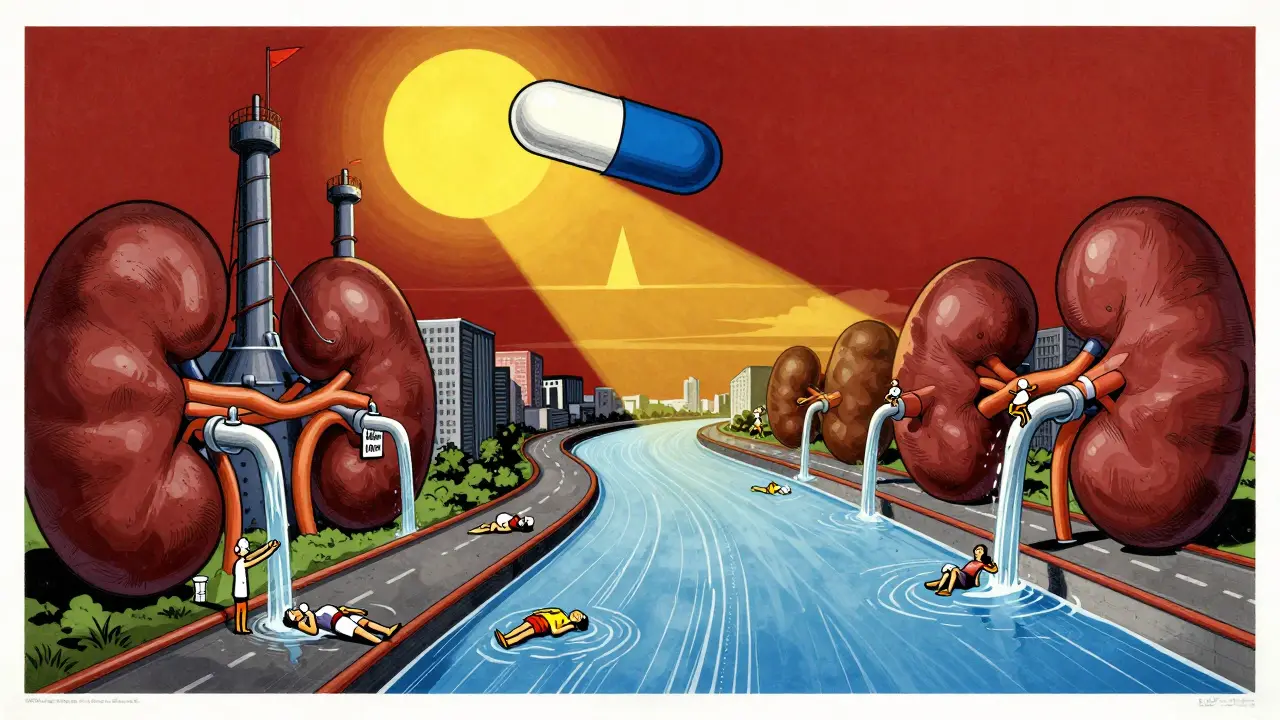
How SGLT2 Inhibitors Work as Diuretics
These drugs block a protein in your kidneys called SGLT2, which normally reabsorbs glucose back into your bloodstream. When it’s blocked, sugar spills into your urine - about 70 to 100 grams per day. But here’s the catch: glucose doesn’t travel alone. It drags sodium and water with it. For every gram of glucose you pee out, you lose about 3.4 mL of water. That adds up to 200-300 mL of extra urine per day, sometimes more. It’s not a strong diuretic like furosemide, but it’s steady. And over time, that steady loss lowers your total blood volume.
This isn’t a bug - it’s a feature. Less fluid in your blood vessels means less pressure on artery walls. That’s why systolic blood pressure drops by 4-6 mmHg on average within two weeks. For someone with high blood pressure, that’s a real win. But for others, especially older adults or those already on blood pressure meds, it can tip them into trouble.
Why Dehydration Happens - And Who’s at Risk
Dehydration from SGLT2 inhibitors doesn’t always mean you’re not drinking enough. It’s about imbalance. Your body is losing fluid faster than you’re replacing it. This is especially common if you’re sick with vomiting or diarrhea, sweating heavily in hot weather, or cutting back on fluids to avoid nighttime bathroom trips.
Studies show that 1.3% to 2.8% of people on these drugs experience volume depletion serious enough to cause symptoms - dry mouth, dark urine, fatigue, or fainting. That’s two to three times higher than placebo. The risk jumps significantly if you’re over 65, have kidney problems (eGFR below 60), or take other diuretics or ACE inhibitors. In one study, patients with baseline systolic blood pressure below 120 mmHg had more than three times the risk of symptomatic low blood pressure.
Real-world reports back this up. On patient forums, people write things like: “I started Jardiance and felt like I was running on empty. My mouth was dry all day, even after drinking.” Another said: “I passed out standing up at the grocery store. My doctor said it was the medication.” These aren’t outliers - they’re predictable outcomes.
Dizziness: The Body’s Warning Signal
Dizziness is the most common symptom tied to this fluid loss. It’s not just “feeling a little off.” It’s lightheadedness when standing, blurred vision, or feeling like you might faint. In clinical trials, 3.5% to 5.8% of users reported dizziness - compared to 2.5% to 3.2% on placebo. That might sound small, but it’s enough to affect daily life.
The timing matters. Most cases show up within the first four weeks, right when your body is adjusting to the fluid shift. About 63% of people who get dizzy also have orthostatic hypotension - meaning their blood pressure drops more than 20 mmHg when they stand up. That’s why standing too fast after sitting or lying down can trigger it.
Age plays a big role. People over 75 are 2.4 times more likely to experience dizziness. So are those taking multiple blood pressure medications. One study found that patients on both an SGLT2 inhibitor and a loop diuretic had a 3.1-fold higher chance of dizziness than those on the SGLT2 drug alone. It’s not the drug itself - it’s the combo.

Blood Pressure Changes: Benefit or Risk?
Lowering blood pressure sounds good - until it goes too low. SGLT2 inhibitors reduce systolic pressure by 4-6 mmHg on average. That’s similar to what you’d get from a low-dose thiazide diuretic. But unlike other diuretics, they don’t cause electrolyte imbalances like low potassium. Instead, they improve arterial stiffness and endothelial function, which may explain why they reduce heart attacks and hospitalizations for heart failure even beyond what you’d expect from BP drops alone.
The catch? If your blood pressure is already low - say, below 110 mmHg systolic - you’re at higher risk. One study found that 12.7% of patients with baseline SBP under 130 mmHg developed orthostatic symptoms, compared to just 4.1% of those with SBP over 140 mmHg. That’s why doctors now check your blood pressure before starting these drugs, especially if you’re older or have heart failure.
For people with heart failure, the trade-off is worth it. The DAPA-HF trial showed dapagliflozin cut cardiovascular death by 17% - saving 6.1 lives per 100 patients over 18 months. But that benefit only holds if you don’t get too dehydrated. So doctors monitor weight, blood pressure, and symptoms closely in the first month.
How to Manage These Side Effects
You don’t have to quit the drug if you feel dizzy or thirsty. There are smart ways to manage it.
- Drink more water - especially in the first few weeks. Add 500-1000 mL (about 2-4 cups) extra daily, even if you don’t feel thirsty. Elderly patients often lose their thirst signal - so don’t wait until you’re dry-mouthed.
- Check your blood pressure standing and sitting - do it at home once a week for the first month. If your systolic drops more than 20 mmHg when you stand, tell your doctor.
- Watch your weight - losing 1.5-2.5 kg in the first week is normal. Losing more than 3 kg? That’s a red flag.
- Hold the dose temporarily if you’re sick with vomiting, diarrhea, or fever. These conditions make fluid loss worse. Resume once you’re eating and drinking normally.
- Don’t rush to stop - most dizziness fades after 2-4 weeks as your body adjusts. If it doesn’t, your doctor might lower the dose (e.g., from 25 mg to 10 mg of empagliflozin) instead of stopping entirely.
Many endocrinologists now recommend starting with a lower dose in high-risk patients - like 10 mg instead of 25 mg of empagliflozin. It cuts side effects without losing much of the benefit.
When to Call Your Doctor
Not every dizzy spell needs an ER visit. But these signs mean it’s time to call:
- Fainting or near-fainting
- Heart racing or chest pain
- Urine output drops below 300 mL/day
- Confusion, extreme fatigue, or muscle cramps
- Weight loss over 3 kg in a week
These could signal severe dehydration or electrolyte imbalance. Don’t wait. Get checked.
Final Thoughts: Weighing the Risks
SGLT2 inhibitors are one of the biggest advances in diabetes care in the last decade. They don’t just lower sugar - they protect your heart and kidneys. But they’re not sugar pills. Their diuretic effect is real, and it comes with trade-offs.
If you’re young, healthy, and active, you’re probably fine. If you’re older, have low blood pressure, or take other diuretics, you need to be careful. Talk to your doctor before starting. Check your blood pressure. Drink water. Monitor your weight. And don’t ignore dizziness - it’s your body telling you something’s off.
For most people, the benefits outweigh the risks. But only if you manage the side effects - not ignore them.
Can SGLT2 inhibitors cause severe dehydration?
Yes, though it’s not common. About 1.3% to 2.8% of users experience volume depletion serious enough to cause symptoms like dizziness, dry mouth, or fainting. Risk increases with age, kidney disease, or use of other diuretics. Hospitalization for dehydration occurs in about 0.8% of patients on higher doses like canagliflozin 300 mg.
Why do I feel dizzy after starting Jardiance or Farxiga?
Dizziness is usually caused by orthostatic hypotension - your blood pressure drops when you stand up. SGLT2 inhibitors reduce blood volume by pulling fluid out through urine. This effect peaks in the first 2-4 weeks. About 63% of people who get dizzy have a systolic drop of 20 mmHg or more when standing. It often improves after your body adjusts.
Do SGLT2 inhibitors lower blood pressure too much?
They typically lower systolic blood pressure by 4-6 mmHg, which is helpful for most people with high blood pressure. But if your blood pressure is already low (below 110-120 mmHg), you’re at higher risk for symptomatic hypotension. Studies show patients with baseline SBP under 130 mmHg are nearly three times more likely to feel dizzy or faint.
Should I stop taking my SGLT2 inhibitor if I get dizzy?
Not necessarily. Most dizziness fades within 2-4 weeks. Instead of stopping, try increasing fluid intake, avoiding sudden standing, and checking your blood pressure at home. If symptoms persist, your doctor may reduce the dose - for example, from 25 mg to 10 mg of empagliflozin - rather than discontinuing the drug entirely, since the heart and kidney benefits are strong.
Are SGLT2 inhibitors safe for elderly patients?
They can be, but extra caution is needed. Older adults (65+) have 2.1 times higher risk of dehydration-related hospitalization. Their thirst sense declines with age, and they’re more likely to be on other blood pressure meds. Experts recommend starting with lower doses, checking orthostatic BP at 1 week, and ensuring adequate hydration. The cardiovascular benefits often still outweigh the risks - if managed properly.
Can I drink alcohol while taking an SGLT2 inhibitor?
Alcohol increases dehydration risk and can worsen dizziness or low blood pressure. It also raises the chance of ketoacidosis, a rare but serious side effect linked to SGLT2 inhibitors. It’s best to limit alcohol, especially during the first few weeks of treatment or if you’re already feeling lightheaded.
What to Do Next
If you’re on an SGLT2 inhibitor and experiencing dizziness or thirst, don’t panic. But don’t ignore it either. Schedule a quick check-in with your doctor. Ask for an orthostatic blood pressure check. Review your other medications - especially diuretics or ACE inhibitors. Adjust your water intake. Track your weight weekly. Most side effects are manageable, and the long-term benefits for your heart and kidneys are significant.
These drugs aren’t perfect. But they’re powerful. And when used wisely, they can change your health trajectory - not just for diabetes, but for life.
