When you have PCOS, losing weight isn't just about eating less or working out more. It’s not laziness. It’s not lack of willpower. It’s biology. And the biggest player in that biology is insulin resistance.
Why PCOS Makes Weight Gain So Hard
Polycystic Ovary Syndrome (PCOS) affects 1 in 10 women of childbearing age. But it’s not just about irregular periods or acne. The real driver behind the stubborn weight gain - especially around the belly - is insulin resistance. This isn’t a side effect. It’s a core feature of PCOS.Insulin is the hormone that tells your cells to take sugar from your blood and use it for energy. In insulin resistance, your cells stop listening. Your pancreas pumps out more insulin to compensate. That extra insulin doesn’t just go to waste. It starts telling your body to store fat - especially in your abdomen. That’s why women with PCOS often develop an "apple shape," not a "pear shape."
Here’s the cycle: high insulin → more fat storage → more insulin resistance → more fat storage. It’s self-reinforcing. And it’s why two women eating the same calories can have wildly different results. One loses weight easily. The other barely moves the needle.
Research shows insulin resistance is present in 70-95% of women with PCOS who are overweight, and even 30-75% of those who are lean. That means you don’t have to be heavy to be affected. Your body’s response to sugar is already broken, even if the scale looks fine.
How Insulin Resistance Fuels PCOS Symptoms
It’s not just about weight. High insulin levels trigger a cascade of hormonal chaos.Insulin tells your ovaries to make more testosterone - the male hormone. Too much testosterone messes with ovulation, causes acne, and leads to unwanted hair growth. At the same time, it lowers SHBG (sex hormone-binding globulin), which normally keeps testosterone in check. So now you’ve got more free testosterone floating around, making everything worse.
And it’s not just hormones. High insulin also increases hunger. It messes with leptin and ghrelin - the hormones that tell you when you’re full or hungry. That’s why women with PCOS often feel insatiable, especially for sugary or carb-heavy foods. Cravings aren’t weakness. They’re a biological signal.
Chronic low-grade inflammation, common in PCOS, makes insulin resistance even worse. Fat tissue, especially around the belly, releases inflammatory chemicals that block insulin’s signal. So you’re stuck in a loop: inflammation → insulin resistance → more belly fat → more inflammation.
The Health Risks You Can’t Ignore
PCOS isn’t just about fertility or appearance. The metabolic risks are serious - and they grow with weight gain.Women with PCOS are up to five times more likely to develop type 2 diabetes. That risk jumps even higher if you’re overweight. High insulin and high blood sugar over time damage blood vessels, raise blood pressure, and spike bad cholesterol (LDL). That’s why heart disease risk is elevated, even in younger women with PCOS.
Abdominal fat is the worst kind. It’s not just stored energy - it’s active tissue that pumps out hormones and inflammatory signals directly into your liver. That’s why waist size matters more than total weight. A waist over 35 inches is a red flag for metabolic trouble.
And it doesn’t stop there. PCOS is linked to sleep apnea, fatty liver disease, and even endometrial cancer due to long-term lack of ovulation and unopposed estrogen. These aren’t distant risks. They’re real, preventable outcomes.
Dietary Strategies That Actually Work
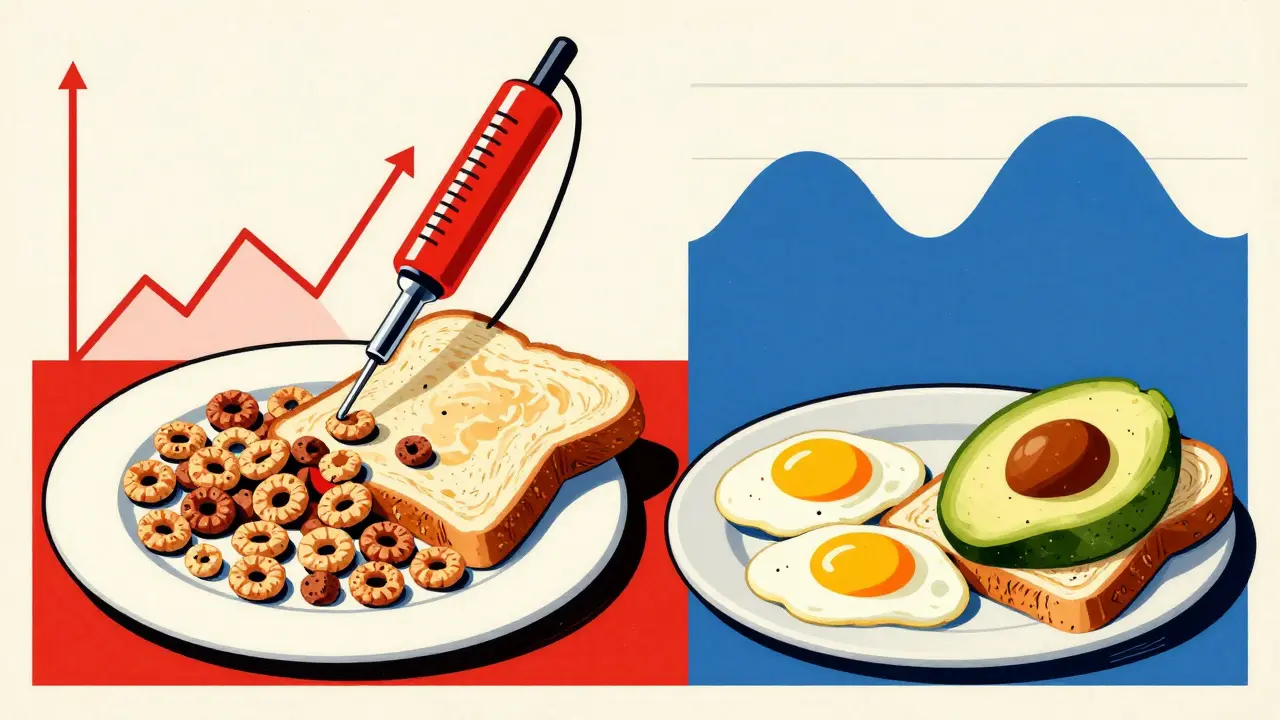
Forget calorie counting. Forget juice cleanses. What works for PCOS is managing insulin - not just for weight loss, but to stop the cycle at its source.1. Lower your carb load - especially refined carbs. White bread, pasta, sugary snacks, and even fruit juices spike insulin fast. Swap them for whole grains, legumes, and non-starchy vegetables. A slice of sourdough is better than white toast. Oats are better than sugary cereal.
2. Pair carbs with protein and fat. Eating a banana alone? Blood sugar spikes. Eating a banana with peanut butter and a handful of almonds? Blood sugar stays steady. That’s because fat and protein slow digestion and blunt insulin spikes.
3. Eat regularly - don’t skip meals. Going too long without eating causes blood sugar to crash, then rebound with intense cravings. Aim for balanced meals every 3-4 hours. Include protein at every meal - eggs, chicken, tofu, beans, fish. Protein helps stabilize insulin and keeps you full.
4. Prioritize fiber. Soluble fiber (found in oats, flaxseed, broccoli, apples) slows glucose absorption and improves insulin sensitivity. Aim for 25-30 grams daily. A cup of lentils gives you 15 grams. That’s half your goal in one meal.
5. Don’t fear natural fats. Avocados, olive oil, nuts, and fatty fish reduce inflammation and improve hormone balance. Healthy fats don’t make you fat - processed carbs and sugar do.
6. Stay hydrated. Dehydration can mimic hunger. Drink water before meals. Sometimes what feels like a craving is just thirst.
What to Avoid
Some "healthy" foods are actually traps for PCOS.- Sugar-free snacks with artificial sweeteners - they can still trigger insulin spikes and cravings.
- Low-fat dairy - often loaded with added sugar to make up for lost flavor.
- Fruit smoothies - blending fruit removes fiber and turns it into a sugar bomb.
- Granola - even "organic" versions are mostly sugar and oil.
- Energy bars - check the label. Many have 20+ grams of sugar.
Real-Life Example: What a PCOS-Friendly Plate Looks Like
Breakfast: Scrambled eggs with spinach, half an avocado, and a slice of whole-grain toast. Lunch: Grilled chicken salad with mixed greens, chickpeas, olive oil, and balsamic vinegar. Snack: A small apple with 1 tablespoon of almond butter. Dinner: Baked salmon, roasted Brussels sprouts, and quinoa. Dessert (optional): A square of dark chocolate (70%+ cocoa). No counting. No deprivation. Just balance.
Weight Loss Isn’t the Only Goal
You don’t need to lose 50 pounds to see improvement. Losing just 5-10% of your body weight can restore ovulation, lower insulin levels, and improve acne and hair growth. That’s not a miracle - it’s science.One study found that women with PCOS who lost 5% of their weight had a 70% improvement in insulin sensitivity. That’s not just about the scale. It’s about getting your periods back, feeling more energy, and reducing your long-term diabetes risk.
And here’s the hopeful part: lifestyle changes can actually change how your genes behave. Epigenetics shows that diet and movement can turn off harmful gene patterns linked to PCOS. You’re not stuck with your biology - you can influence it.
When Diet Isn’t Enough
Diet is powerful, but it’s not magic. Some women need medication - like metformin - to help their bodies respond to insulin better. That’s not a failure. It’s support. Talk to your doctor. Medication can make dietary changes more effective.Also, sleep and stress matter. Poor sleep raises cortisol, which worsens insulin resistance. Chronic stress triggers emotional eating. Prioritize 7-8 hours of sleep. Try walking, yoga, or deep breathing. You don’t need to meditate for an hour. Five minutes of slow breathing counts.
Final Thought: This Is Not About Perfection
You don’t need to eat perfectly. You need to eat consistently. One sugary meal won’t ruin everything. But if you’re eating them every day, the cycle keeps going.Start small. Swap one processed snack for a handful of nuts. Drink water before lunch. Add one serving of vegetables to dinner. Build from there.
PCOS makes weight harder - but it doesn’t make it impossible. The same insulin resistance that stores fat can be trained to stop. And when it does, everything else starts to improve.
Can you have PCOS and still be thin?
Yes. While PCOS is often linked with weight gain, up to 30-75% of women with PCOS are lean or of normal weight. Insulin resistance still occurs in these cases - it just doesn’t show up as visible fat. The hormonal imbalance and metabolic issues remain, and can still cause irregular periods, acne, and fertility challenges. Weight isn’t the only indicator.
Why do I crave sugar so badly with PCOS?
High insulin levels mess with your hunger hormones. They lower leptin (the full signal) and raise ghrelin (the hunger signal). At the same time, insulin spikes cause blood sugar to crash, triggering intense cravings for quick energy - sugar. It’s not willpower. It’s biology. Eating protein and fat with carbs helps stabilize this.
Is a low-carb diet the best option for PCOS?
A moderate low-carb diet works best for most women with PCOS - not a zero-carb extreme. Cutting out refined carbs and sugars is key. But whole grains, legumes, and starchy vegetables (like sweet potatoes) are fine in controlled portions. They provide fiber and nutrients that support insulin sensitivity. The goal is steady blood sugar, not zero carbs.
Will losing weight cure PCOS?
No - PCOS is a lifelong condition. But losing even 5-10% of body weight can dramatically improve symptoms. Many women resume regular periods, reduce acne and hair growth, and lower their risk of diabetes. It doesn’t "cure" PCOS, but it reverses its worst effects. That’s a huge win.
Does exercise help with PCOS weight gain?
Yes - but not in the way you think. You don’t need to run marathons. Strength training and moderate cardio (like brisk walking or cycling) improve insulin sensitivity more than intense workouts. Muscle tissue uses glucose without insulin. Building muscle helps your body manage sugar better. Consistency matters more than intensity.