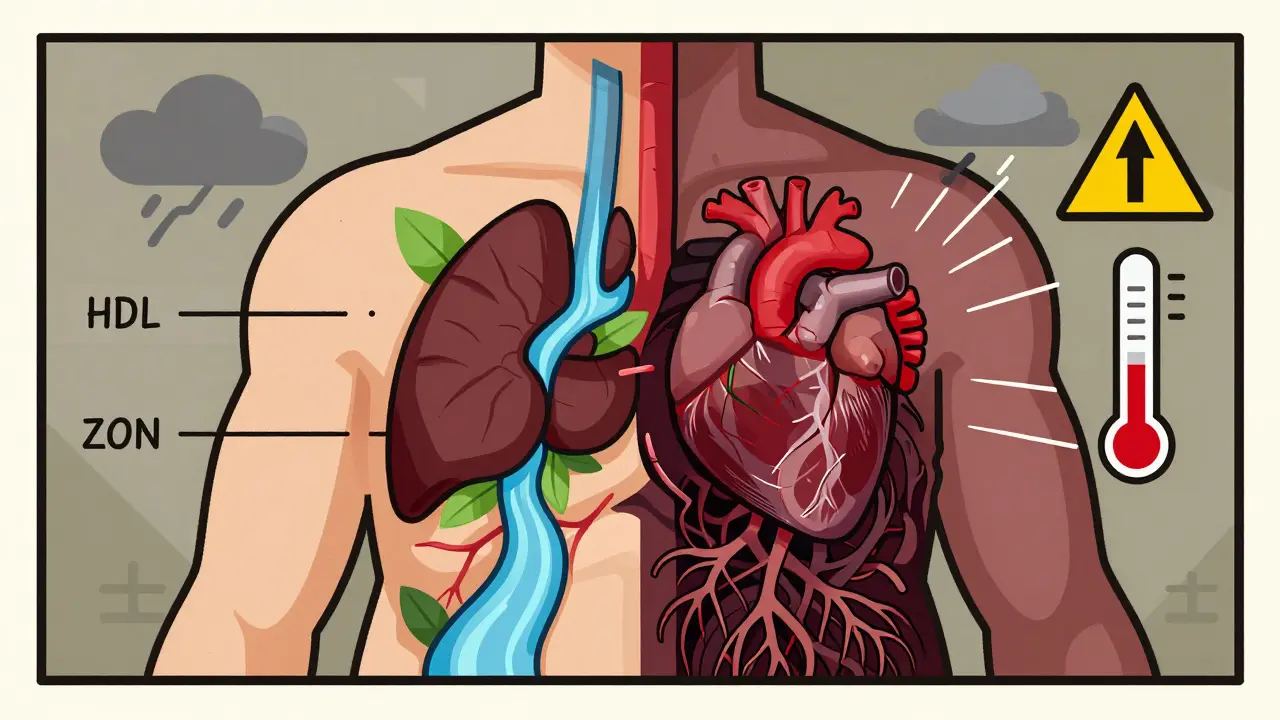
Metabolic syndrome isn't a single disease. It’s a warning sign-a cluster of five interconnected risk factors that, when they show up together, dramatically increase your chances of having a heart attack, stroke, or developing type 2 diabetes. Think of it like a storm system: high blood pressure, excess belly fat, abnormal cholesterol, and elevated blood sugar don’t just add up-they multiply each other’s damage. And right now, nearly 1 in 3 American adults has it.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome is diagnosed when you have at least three of these five specific conditions:- Waist circumference over 40 inches for men, or 35 inches for women (lower for Asian Americans: 35 inches for men, 31 inches for women)
- Triglycerides at or above 150 mg/dL
- HDL cholesterol below 40 mg/dL for men, or below 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar at or above 100 mg/dL
It’s not enough to have one or two of these. The real danger kicks in when three or more show up at once. That’s when your risk of heart disease jumps by 50% to 100%, and your chance of getting type 2 diabetes goes up five times.
What ties all these together? Insulin resistance. That’s when your body’s cells stop responding properly to insulin-the hormone that shuttles sugar from your blood into your muscles and fat for energy. Your pancreas tries to compensate by pumping out more insulin, but over time, this backfires. High insulin levels start to raise blood pressure, mess with fat storage, and lower good cholesterol. The result? A perfect storm inside your body.
Why Belly Fat Is the Core Problem
Not all fat is the same. Fat under your skin (subcutaneous) is mostly harmless. But fat packed around your organs-visceral fat-is the real troublemaker. That’s what the waist measurement is really tracking.Visceral fat isn’t just sitting there. It’s active. It releases inflammatory chemicals and free fatty acids directly into your liver, which then ramps up bad cholesterol production and blocks insulin from working. This is why someone with a 42-inch waist but normal weight on the scale can still have metabolic syndrome. The scale doesn’t tell you where the fat is.
Studies show that people with excess belly fat-even if they’re not overweight-have significantly higher rates of heart disease than those with fat distributed elsewhere. That’s why doctors now measure waist size as carefully as blood pressure.
The Hidden Cost: Why Most People Don’t Know They Have It
Here’s the scary part: most people with metabolic syndrome don’t feel sick. No chest pain. No dizziness. No obvious symptoms. That’s why it flies under the radar.A survey of over 1,200 patients found that nearly 7 out of 10 had no idea they had metabolic syndrome-even though they’d been diagnosed with high blood pressure, high cholesterol, or prediabetes. Doctors often treat each piece separately: one pill for blood pressure, another for cholesterol, maybe a glucose-lowering drug. But rarely do they connect the dots.
That’s a problem because treating each factor alone doesn’t stop the underlying driver: insulin resistance. You can take a statin and still be at high risk if your belly fat keeps growing and your blood sugar stays elevated.

It’s Not Just About Diet and Exercise-It’s About System Change
The good news? Metabolic syndrome can be reversed. The bad news? Pills won’t fix it.The landmark Diabetes Prevention Program showed that people who lost 7% of their body weight and walked 150 minutes a week cut their risk of developing diabetes by 58%. That same lifestyle change also reversed metabolic syndrome in 41% of participants over 10 years.
But here’s what most people don’t realize: it’s not about going on a diet. It’s about changing how you live. That means:
- Swapping sugary drinks for water or unsweetened tea
- Eating more vegetables, beans, and whole grains instead of processed carbs
- Getting up and moving every hour-especially if you sit all day
- Getting enough sleep (less than 6 hours a night worsens insulin resistance)
- Managing stress-chronic stress raises cortisol, which promotes belly fat storage
People who succeed don’t do it alone. They work with dietitians, exercise physiologists, and behavioral coaches. The Mayo Clinic’s program, for example, had 68% of participants reverse their metabolic syndrome after a year of structured support.
Why Some People Struggle More Than Others
Not everyone has the same fight. Women with polycystic ovary syndrome (PCOS) often battle severe insulin resistance, making weight loss harder despite strict diets. Older adults may lose muscle mass, slowing metabolism. People in low-income communities face food deserts, unsafe neighborhoods for walking, and lack of access to specialists.Studies show that community health workers-people from the same neighborhoods as the patients-are more effective than traditional clinics at helping people lose weight. In one CDC program, Hispanic participants coached by lay health educators lost nearly 6% of their body weight, compared to just over 4% with standard care.
Insurance is another barrier. Only about 1 in 4 Medicare Advantage plans fully cover evidence-based lifestyle programs. If you’re paying out of pocket, a 12-month program can cost $1,000 or more-unless your employer or local health department offers it for free.
New Tools Are Changing the Game
Technology is starting to help. In January 2023, the FDA approved the first digital therapeutic app for metabolic syndrome: DarioHealth’s Metabolic+. It uses continuous glucose monitoring to show users how their meals affect blood sugar in real time, paired with daily coaching.In a clinical trial, users saw their HbA1c (a measure of long-term blood sugar) drop by 0.6% and their waist size shrink by over 1 inch in just six months. That’s not just a number-it’s a sign that insulin resistance is improving.
Doctors are also starting to use genetic testing to predict who responds best to certain diets. Some people lose weight better on low-carb diets; others do better on high-fiber, plant-based plans. The right match makes all the difference.

What Happens If You Do Nothing?
Left untreated, metabolic syndrome doesn’t stay stable. It progresses.Over 75% of new type 2 diabetes cases are directly linked to metabolic syndrome. And once diabetes sets in, your risk of heart disease doubles again. The economic toll is staggering: heart disease and stroke caused by metabolic syndrome cost the U.S. over $360 billion a year.
And it’s getting worse. Since 2000, the number of Americans with metabolic syndrome has climbed 35%. By 2030, nearly 4 in 10 adults globally may have it-especially in countries where fast food and sedentary jobs are becoming the norm.
You Can Turn This Around-Here’s How to Start Today
You don’t need a miracle. You need a plan.- Measure your waist. If you’re a man over 40 inches or a woman over 35 inches, you’re at risk-even if your BMI is normal.
- Ask for a fasting glucose and lipid panel. Don’t wait for symptoms. Get your numbers checked if you’re over 40, overweight, or have a family history of diabetes or heart disease.
- Start walking. Thirty minutes a day, five days a week. That’s it. No gym needed.
- Swap one sugary item per day. Replace soda with sparkling water. Swap cereal for eggs and veggies. Small changes add up.
- Find support. Look for a local Diabetes Prevention Program. Many are free through hospitals or the CDC.
Metabolic syndrome isn’t a life sentence. It’s a signal. A chance to change course before your heart pays the price. The science is clear: lifestyle works better than any drug. And the sooner you start, the more you can undo.
Can you have metabolic syndrome and still be thin?
Yes. While obesity is a major risk factor, some people carry excess fat around their organs even if they appear slim on the scale. This is called TOFI-thin on the outside, fat inside. A waist measurement over 40 inches for men or 35 inches for women is a stronger indicator than body weight alone. Blood tests for triglycerides, HDL, and fasting glucose are needed to confirm.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one of five possible components. You can have prediabetes without metabolic syndrome, and you can have metabolic syndrome without prediabetes-if you have three other risk factors like high blood pressure, low HDL, and large waist size.
Do I need medication for metabolic syndrome?
Medication isn’t the first line of defense. Lifestyle changes are proven to reverse the condition. But if your blood pressure, cholesterol, or blood sugar is dangerously high, your doctor may prescribe pills to reduce immediate risk while you work on long-term changes. There’s no drug approved specifically to treat metabolic syndrome as a whole-only its individual parts.
How long does it take to reverse metabolic syndrome?
Many people see improvements in as little as 6 months. Losing just 5-7% of your body weight can lower blood pressure, improve cholesterol, and bring blood sugar down. Studies show that with consistent lifestyle changes, up to 70% of people can reverse the diagnosis within a year. The key is consistency-not perfection.
Can children get metabolic syndrome?
Yes. With rising childhood obesity, metabolic syndrome is now common in teens, especially those with a family history of diabetes or heart disease. Doctors use adjusted waist and blood pressure thresholds for children. Early intervention with diet, activity, and sleep habits can prevent lifelong complications.
Does alcohol affect metabolic syndrome?
Moderate alcohol (one drink a day for women, two for men) may slightly raise HDL, but it also adds empty calories and can increase triglycerides. For people with metabolic syndrome, alcohol can worsen insulin resistance and liver fat buildup. Cutting back or eliminating alcohol is often part of successful treatment plans.