LAI Side Effect Monitoring Tool
LAI Monitoring Requirements
Olanzapine LAI (Zyprexa Relprevv)
Key Side Effects: Weight gain, diabetes, sedation, post-injection delirium
Required Monitoring Frequency: Before and after every injection
Special Protocol: 3-hour mandatory observation; black box warning
Why this matters: Olanzapine has the highest risk of severe metabolic side effects and carries a black box warning requiring 3-hour observation after injection.
Long-acting injectables are changing how we treat serious mental illness - but only if we monitor them properly
For people living with schizophrenia or other severe psychiatric conditions, long-acting injectables (LAIs) can be life-changing. Instead of swallowing pills every day, patients get a shot every few weeks or even every few months. It sounds simple. But behind that convenience is a complex web of physical risks that many clinics are ignoring. The data doesn’t lie: only 45% of patients on LAIs have their side effects properly tracked in a year. That means more than half are walking around with unmonitored weight gain, high blood sugar, abnormal movements, or even life-threatening reactions - all while their doctors focus on whether they’re "feeling better." This isn’t negligence. It’s a system failure.
LAIs aren’t magic bullets. They’re powerful drugs with serious, sometimes delayed, consequences. And because they stay in your body for weeks, side effects don’t show up right away. They creep in. A patient might gain 10 pounds over three months and not realize it’s the medication. Their cholesterol might spike. Their blood pressure might climb. Their hands might start twitching. But if no one checks, no one acts. And that’s when mental health care becomes dangerous.
What LAIs really do - and what they hide
Long-acting injectables work by slowly releasing antipsychotic medication into the bloodstream over time. The most common ones include paliperidone (Invega Sustenna), aripiprazole (Abilify Maintena), olanzapine (Zyprexa Relprevv), and haloperidol. Each has different risks. Olanzapine, for example, is known for causing rapid weight gain and high blood sugar - and it comes with a black box warning that requires a mandatory 3-hour observation after every injection because of rare but deadly reactions. Paliperidone can spike prolactin levels, leading to sexual dysfunction, breast milk production, or bone loss. Aripiprazole might cause akathisia - a terrifying inner restlessness that can make people feel like they’re crawling out of their skin.
And these aren’t rare side effects. FDA data shows that 20-30% of patients on LAIs develop metabolic syndrome - a cluster of conditions including obesity, high blood pressure, and insulin resistance that dramatically increases heart disease risk. One study found patients gained an average of 4.2 kilograms in just six months. That’s not a side effect. That’s a health crisis.
First-generation LAIs like haloperidol are even worse. Up to 50% of users develop extrapyramidal symptoms - uncontrollable muscle spasms, tremors, and stiffness. These can become permanent. Tardive dyskinesia, a condition where people develop involuntary facial movements, affects 10-20% of long-term users. And once it starts, it rarely goes away.
The monitoring gap: Where clinics are falling short
Here’s the shocking part: every single patient getting an LAI injection has a scheduled appointment. That’s a built-in opportunity to check their health. But in 2021, a major audit of 5,169 patients across 62 UK mental health services found that only 45% had any documented side effect assessment. Let that sink in. More than half weren’t checked for weight, blood pressure, blood sugar, or movement disorders - even though they were getting injections every month.
Even worse, the specific checks were even rarer:
- Weight checks: 38% of patients
- Blood pressure monitoring: 32%
- Metabolic panels (glucose and lipids): just 15%
Why? Time. Money. Training. Most clinics have 15-minute slots for injections. Clinicians prioritize whether the patient’s hallucinations are under control - not whether their liver is failing. One community psychiatrist on Reddit put it bluntly: "I have 15 LAI patients but only 15 minutes per appointment - I prioritize symptoms over side effects because that’s what gets reimbursed."
Meanwhile, 62% of mental health nurses surveyed in 2023 said they lacked proper training on how to spot LAI side effects. Most were taught to look for redness at the injection site - not for signs of neuroleptic malignant syndrome, a rare but deadly reaction that can cause fever, muscle rigidity, and organ failure.

How different LAIs demand different monitoring
Not all LAIs are created equal. Each one needs its own monitoring plan. Here’s how they compare:
| Medication | Key Side Effects | Required Monitoring Frequency | Special Protocol |
|---|---|---|---|
| Olanzapine LAI (Zyprexa Relprevv) | Weight gain, diabetes, sedation, post-injection delirium | Before and after every injection | 3-hour mandatory observation; black box warning |
| Paliperidone LAI (Invega Sustenna) | Prolactin elevation, metabolic syndrome, sexual dysfunction | Every 3 months | Check prolactin levels, fasting glucose, lipids |
| Aripiprazole LAI (Abilify Maintena) | Akathisia, insomnia, weight gain (milder) | Every 3 months | Use AIMS scale monthly for restlessness |
| Haloperidol LAI | Extrapyramidal symptoms, dystonia, tardive dyskinesia | Monthly | AIMS scale every 3 months; frequent neurological exams |
Paliperidone causes the highest rates of weight gain and high prolactin. Aripiprazole has fewer metabolic risks but causes more inner restlessness. Olanzapine? It’s the most dangerous - and requires the most oversight. Yet many clinics treat them all the same. That’s like giving the same follow-up care to someone with a broken leg and someone with a heart condition.
What proper monitoring looks like - and how it saves lives
There’s a better way. The National Council’s 2022 guide outlines a clear protocol:
- Pre-injection check (5-10 minutes): Measure weight, waist size, blood pressure, and heart rate. Ask about movement issues, mood changes, sexual function, and sleep.
- Post-injection observation: Stay with the patient for at least 30 minutes. For olanzapine? Three full hours.
- Quarterly AIMS test: Use the Abnormal Involuntary Movement Scale to check for tremors or twitching.
- Every 6 months: Run a full metabolic panel - fasting glucose, cholesterol, triglycerides.
- Document everything: If it’s not written down, it didn’t happen.
When clinics followed this model, hospitalizations dropped by 40%. Why? Because problems were caught early. A patient’s blood sugar started rising? They got a referral to a dietitian. Their movement disorder worsened? Their dose was adjusted. Their blood pressure spiked? They started a safe medication.
One 2022 case study from a community center showed that after implementing full monitoring, patients stayed on their LAIs longer, had fewer emergency room visits, and reported better quality of life. That’s not just good care - it’s cost-effective care. A 2021 analysis found that adding 15-20 minutes per visit cut long-term costs by 25% by preventing hospitalizations.
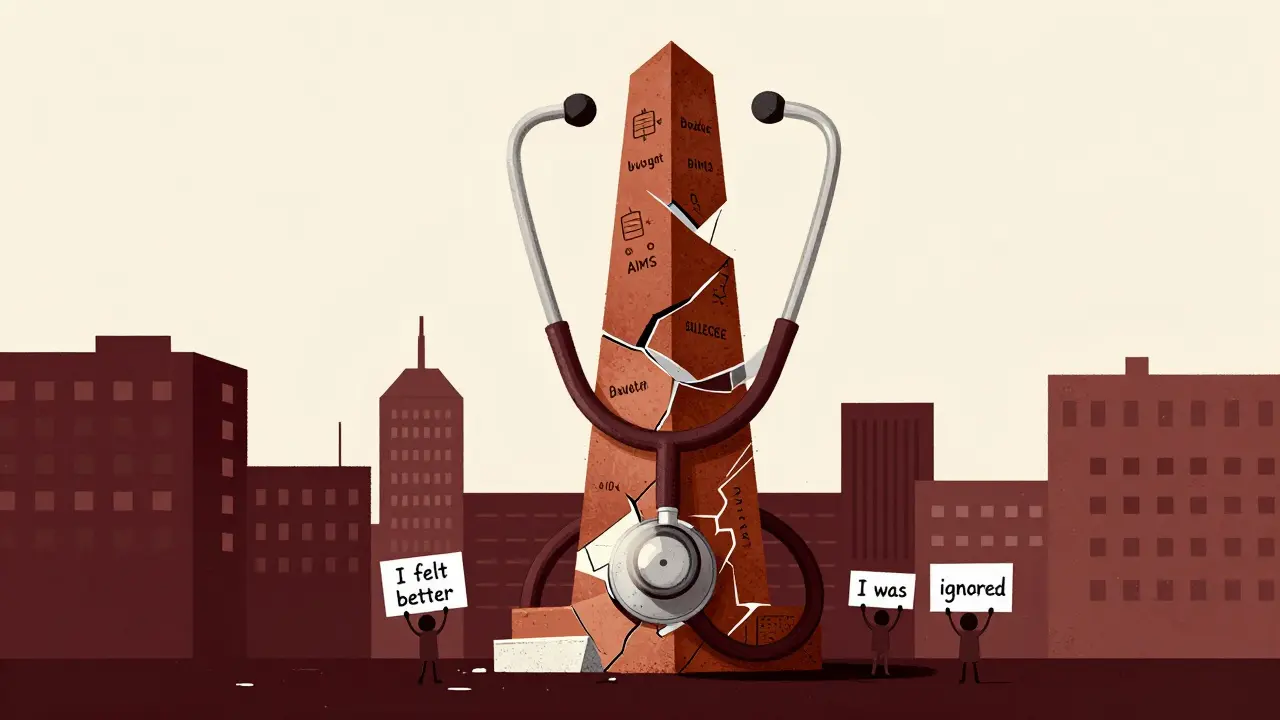
The human cost of ignoring monitoring
Patients aren’t just statistics. One user on Schizophrenia.com shared: "I gained 30 pounds on Invega Sustenna over 18 months before anyone checked my metabolic panel. My doctor just asked, ‘How are you feeling mentally?’" That’s the story too many people live.
On the flip side, those with consistent monitoring report feeling safer. One woman said, "They checked my weight every time. When I started gaining, they switched my med. I didn’t feel like a lab rat - I felt like someone cared."
When monitoring is ignored, side effects become invisible. Weight gain turns into shame. Movement disorders turn into isolation. High blood sugar turns into diabetes. And when those conditions worsen, patients often stop taking their medication - not because they want to, but because they feel worse physically than mentally.
What’s changing - and what’s still broken
There’s progress. In 2023, 68% of U.S. mental health systems had some kind of LAI monitoring protocol - up from 42% in 2020. Medicare Advantage plans are now tying reimbursement to monitoring quality. Digital tools are emerging: apps that remind patients to log symptoms between visits, telehealth check-ins for weight and blood pressure.
But only 22% of clinics meet all the recommended standards. And the biggest gap? Training. Nurses and clinicians still aren’t taught how to do this. The American Association of Psychiatric Pharmacists says staff need 8-16 hours of specialized training just to assess movement disorders. Most don’t get it.
And here’s the kicker: the LAI market is growing. It’s worth $5.8 billion and will hit $35% of all antipsychotic prescriptions by 2030. But if we don’t fix monitoring now, we’re not just failing patients - we’re building a public health time bomb.
What needs to change - and how
It’s not rocket science. We need:
- Standardized protocols: Every clinic should follow the same checklist - no exceptions.
- Reimbursement reform: Insurance must pay for monitoring time. Right now, doctors get paid for the injection, not for checking your blood sugar.
- Training mandates: All staff administering LAIs need certified training in side effect recognition.
- Technology integration: Use apps to collect patient-reported symptoms between visits. Combine them with clinic data.
- Accountability: Track monitoring rates like we track infection rates in hospitals. Publish them. Shame the low performers.
Long-acting injectables are one of the most promising tools we have for treating serious mental illness. But they’re not a shortcut. They’re a responsibility. Every injection is a chance to protect someone’s body - not just their mind. If we keep treating them like a simple shot, we’ll keep losing people to preventable complications. The science is clear. The data is clear. Now we just need the will to act.