When a patient in a nursing home is switched from one blood thinner to another-without their doctor’s direct order-it’s not a mistake. It’s policy. This is how institutional formularies work: they let pharmacists replace prescribed drugs with alternatives that are cheaper, equally effective, and approved by the facility’s own rules. These systems aren’t just about saving money. They’re designed to reduce errors, prevent dangerous drug interactions, and make sure every patient gets the right treatment. But they also create confusion, especially when patients move between hospitals, clinics, and nursing homes. Understanding how these formularies operate is critical for anyone navigating today’s healthcare system.
What Exactly Is an Institutional Formulary?
An institutional formulary is a living list of approved medications that a hospital, nursing home, or clinic allows its staff to use. It’s not a static catalog. It’s updated regularly based on new research, cost changes, and real-world patient outcomes. Unlike insurance formularies-which decide what drugs your plan will pay for-institutional formularies control what drugs can be given to patients within a specific facility. The key difference? Institutional formularies allow for therapeutic substitution: swapping one drug for another that’s chemically different but expected to work the same way. For example, switching from brand-name Xarelto to generic apixaban for blood clot prevention. This practice is legally defined and tightly regulated. In Florida, Statute 400.143 (2025) spells out exactly how it must be done. Facilities must have a committee made up of the medical director, director of nursing, and a certified consultant pharmacist. This group writes the rules, picks which drugs go on the list, and tracks what happens after substitutions are made. The goal isn’t to limit care-it’s to make sure care is safe, consistent, and cost-effective.How Therapeutic Substitution Works in Practice
Therapeutic substitution doesn’t happen randomly. It follows a strict process. A patient is admitted to a nursing home on warfarin, for example. The facility’s formulary lists apixaban as the preferred option because it’s easier to monitor, has fewer food interactions, and costs less. The pharmacist, following approved guidelines, switches the medication. But here’s the catch: the change must be documented, the prescriber must be notified, and the patient’s response must be tracked. Most formularies use a tiered system. Tier 1 includes the most cost-effective, evidence-backed drugs-usually generics. Patients pay the least out of pocket for these. Tier 2 and 3 include brand-name or newer drugs that offer marginal benefits but cost significantly more. Getting a drug from Tier 3 often requires a prior authorization, which can delay treatment. This structure pushes providers toward the best value options, but it also creates friction. In a 2024 survey of Florida nursing homes, staff reported that therapeutic substitution helped catch seven previously undetected drug interactions in the first year alone. That’s a win for safety. But another pharmacist on Reddit shared a frustrating case: a patient was switched to apixaban in a nursing home, then sent back to the hospital where they were immediately switched back to Xarelto. No one told the hospital team about the change. The patient got confused. The family panicked. The medical record didn’t reflect the substitution. That’s the downside: poor communication across settings.Who Decides What Goes on the Formulary?
It’s not a single doctor or administrator making these calls. It’s a committee. Florida law requires three key members: the medical director (who understands clinical needs), the director of nursing services (who sees how drugs are administered daily), and a certified consultant pharmacist (who knows drug interactions, bioequivalence, and dosing nuances). This mix ensures decisions aren’t made by cost alone-or by clinical preference alone. The committee uses evidence-based guidelines from sources like the American Society of Health-System Pharmacists (ASHP) and the Academy of Managed Care Pharmacy (AMCP). They review clinical trials, real-world outcomes, and cost data. A drug doesn’t make the list just because it’s popular. It has to prove it delivers better or equal results at a lower price. For example, generic metformin replaced brand-name Glucophage across most U.S. hospitals years ago-not because Glucophage was unsafe, but because the generic worked just as well and cost 90% less. These committees meet quarterly to review new drugs, remove ineffective ones, and assess whether substitutions are working. They track things like readmission rates, adverse events, and patient satisfaction. If a substituted drug leads to more hospital visits, it gets pulled. If a new generic shows better outcomes, it gets added. This isn’t bureaucracy-it’s continuous quality improvement.Formularies vs. Insurance Plans: Key Differences
People often confuse institutional formularies with insurance formularies. They’re related but serve different purposes. Insurance formularies determine what your health plan will cover and how much you pay for each drug. If your plan doesn’t cover a drug, you pay full price-or get denied. Institutional formularies determine what drugs a hospital or nursing home will stock and use. A patient might have a drug on their insurance formulary but not on their nursing home’s institutional formulary. That’s common. The insurance plan might cover brand-name Lisinopril, but the facility’s formulary only stocks the generic because it’s cheaper and just as effective. The pharmacist can still substitute it-without asking the patient or doctor-because the facility’s policy allows it. This creates a gap in care. A patient discharged from a nursing home might go home on a substituted drug, but their primary care doctor isn’t told about the change. The doctor keeps prescribing the original drug. The pharmacy fills it. The patient ends up taking two drugs that do the same thing. That’s how errors happen.Real-World Impact: Benefits and Risks
Studies show institutional formularies reduce adverse drug events by 15-30%. In long-term care settings, where patients often take five or more medications, that’s huge. One Florida facility found that after implementing its formulary, the number of falls linked to sedatives dropped by 40% in six months. Why? They replaced high-risk benzodiazepines with safer alternatives. But there’s a flip side. A 2023 AMA survey found that 78% of physicians feel formularies create bureaucratic hurdles. Getting approval for a non-formulary drug can take days. For a patient with complex heart failure or rare epilepsy, that delay can be dangerous. Some drugs simply don’t have good generic alternatives. Others work better for certain genetic profiles. Formularies don’t always account for that. Patients, especially older adults, often don’t know they’ve been switched. AARP reports that many residents in nursing homes aren’t told about substitutions, so they can’t ask questions or report side effects. That’s a consent issue. If a patient’s blood pressure drops after a switch, they might think it’s just aging-not a drug reaction.Implementation Challenges and Solutions
Setting up a formulary isn’t easy. Florida requires facilities to establish their committee within 90 days of starting the program. Staff need training. Electronic health records (EHRs) must be updated to flag substitutions. Sixty-eight percent of facilities in a 2024 state survey reported initial EHR integration problems. Solutions are emerging. Some hospitals now use automated alerts in their EHR systems. When a pharmacist makes a substitution, the system automatically notifies the prescriber, updates the medication list, and sends a summary to the patient’s primary care provider. That’s a big improvement. Others use standardized substitution protocols that list exactly which drugs can be swapped-and under what conditions. Training is critical. Nurses, who administer most medications, need to understand why substitutions happen. Pharmacists need to know how to document them clearly. Administrators need to track outcomes-not just compliance. The average facility spends 20-30 hours per quarter just maintaining its formulary records.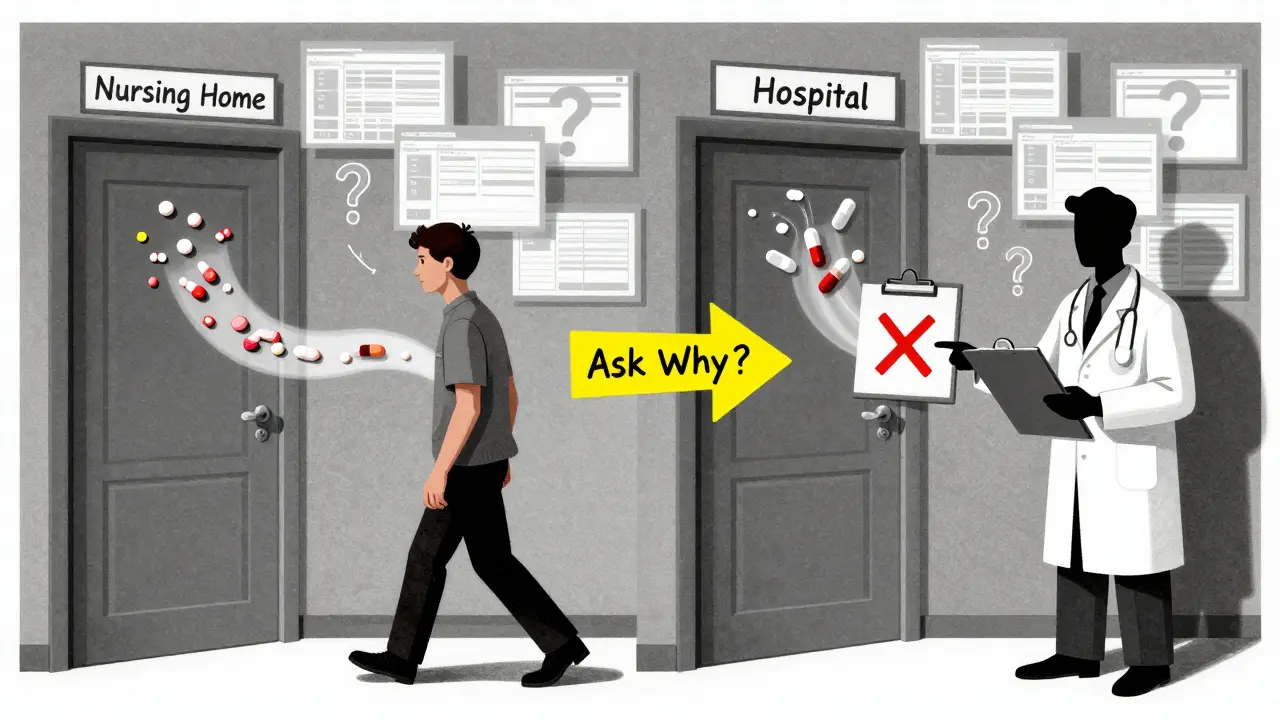
The Future: AI, Genomics, and More Transparency
The next wave of formulary management is smarter. By 2026, Gartner predicts 80% of healthcare systems will use AI to adjust formularies in real time based on patient outcomes. If a group of patients on a certain drug starts having more kidney issues, the system flags it and suggests alternatives-even before a committee meets. Pharmacogenomics is also entering the picture. Some hospitals are starting to test patients for genetic variants that affect how they metabolize drugs. If someone is a slow metabolizer of clopidogrel, for example, they won’t respond well to it. Formularies can then automatically exclude it for that patient and recommend a better alternative. The federal government is pushing for change too. CMS plans to include institutional formulary compliance in Nursing Home Compare ratings starting in late 2025. That means facilities with poor substitution tracking could lose funding or public trust. The FDA is also working on a 2025 pilot to standardize therapeutic equivalence ratings across more drug classes. Right now, only about 60% of medications have clear equivalence designations. More clarity means fewer debates, fewer errors, and better substitutions.What Patients and Families Should Know
If you or a loved one is in a hospital, nursing home, or clinic, here’s what to do:- Ask: “Is this the same drug my doctor prescribed?”
- Ask: “Why was it changed?”
- Ask: “Can I get the original drug if I prefer it?”
- Keep your own list of medications-and update it every time a change is made.
- Make sure your primary care doctor gets a copy of your discharge summary, including any substitutions.
Conclusion: Formularies Are Tools-Not Rules
Institutional formularies aren’t perfect. They can create confusion, delay care, and leave patients in the dark. But they also save lives. They prevent dangerous drug interactions. They reduce waste. They make sure the right drug is used for the right patient. The key is balance: evidence-based decisions, clear communication, and patient-centered care. The future of healthcare isn’t about eliminating formularies. It’s about making them smarter, more transparent, and more responsive to individual needs. Until then, staying informed is your best defense.What is therapeutic substitution in a hospital or clinic?
Therapeutic substitution is when a pharmacist replaces a prescribed drug with a different drug that is expected to have the same clinical effect. For example, switching from brand-name Xarelto to generic apixaban for blood clot prevention. This is allowed under institutional formulary policies, as long as it follows approved guidelines and is documented properly.
Are institutional formularies the same as insurance formularies?
No. Insurance formularies determine what drugs your health plan will cover and how much you pay. Institutional formularies determine what drugs a hospital, nursing home, or clinic will stock and use. A drug can be covered by your insurance but not available at the facility-and vice versa.
Why do hospitals switch medications without asking the patient?
Hospitals follow institutional formulary policies that allow pharmacists to substitute drugs to improve safety and reduce costs. These substitutions are based on clinical evidence and are often made to avoid dangerous interactions or to use more cost-effective generics. But patients should still be informed-many facilities don’t do this well.
Can I refuse a drug substitution?
Yes. You have the right to refuse any substitution if you understand the reason and potential risks. If you prefer the original medication, you can ask for it. Some facilities may require a signed form or a note from your doctor, but you can’t be forced to accept a substitute.
How often are institutional formularies updated?
Formularies must be reviewed and updated at least annually, but many facilities review them quarterly or even monthly. In Florida, facilities are required to monitor therapeutic substitution outcomes every three months. Updates are based on new clinical data, drug safety alerts, cost changes, and patient outcomes.
What’s the role of a consultant pharmacist in institutional formularies?
A consultant pharmacist, certified under state law, is responsible for evaluating drug effectiveness, identifying potential interactions, and ensuring substitutions follow evidence-based standards. They bring specialized knowledge about pharmacology and medication safety that doctors and nurses may not have. In Florida, they’re a required member of the formulary committee.
Do institutional formularies apply to all hospitals?
Not all, but most. As of 2024, 94% of nursing homes in the U.S. use formal institutional formularies. About 78% of acute care hospitals do. States like Florida have strict laws requiring them, while others leave it up to individual facilities. The trend is toward universal adoption, especially as payers and regulators tie reimbursement to formulary compliance.
