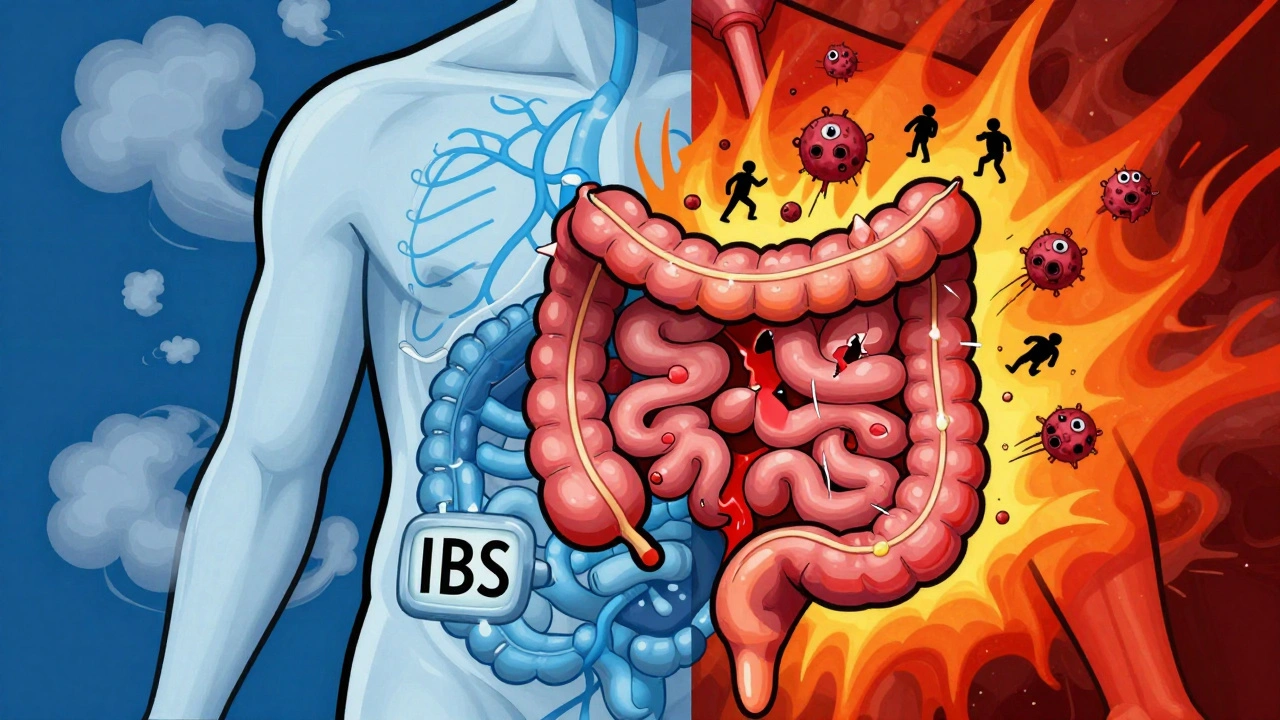
Many people think IBS and IBD are the same thing-just bad digestion. But they’re not. One is a malfunctioning system with no visible damage. The other is a disease that physically tears your gut apart. Confusing them can delay real treatment-or worse, make you ignore life-threatening signs.
What Is IBS? It’s Not in Your Head-It’s in Your Gut’s Wiring
IBS, or Irritable Bowel Syndrome, doesn’t show up on scans, blood tests, or colonoscopies. Your intestines look perfectly normal. But they don’t work right. It’s like your gut’s nervous system got stuck in overdrive. You feel pain, bloating, and sudden urges-but there’s no ulcer, no swelling, no scar tissue.
The Rome IV criteria, used by doctors worldwide since 2016, define IBS by three things: abdominal pain at least once a week for three months, plus two of these: improvement after a bowel movement, changes in stool frequency, or changes in stool appearance. About 76% of people with IBS report constant bloating. Nearly half see mucus in their stool. And most notice symptoms flare up after eating.
There’s no inflammation. No damage. No cancer risk. That’s why doctors call it a functional disorder. It’s not broken-it’s misfiring. Think of it like a faulty thermostat in your house. The heater works fine, but it turns on when it shouldn’t. That’s IBS.
What Is IBD? Your Body Is Fighting Itself
IBD-Inflammatory Bowel Disease-isn’t just discomfort. It’s autoimmune destruction. Your immune system attacks your own digestive tract, causing chronic inflammation, open sores, and scarring. The two main types are Crohn’s disease and ulcerative colitis.
Crohn’s can hit anywhere from mouth to anus, chewing through all layers of the bowel wall. Ulcerative colitis sticks to the colon and rectum, eating away at the inner lining. In both, inflammation is constant. And it shows up everywhere: in blood tests, stool samples, and most importantly-inside your gut during a colonoscopy.
Doctors see ulcers, bleeding, strictures (narrowed sections), and fistulas (abnormal tunnels between organs). Up to 92% of ulcerative colitis patients have blood in their stool. About 65% of IBD patients lose weight without trying. Fever? That’s not normal for IBS. It’s a red flag for IBD.
And it gets worse. IBD can lead to colorectal cancer after 10+ years of pancolitis. Toxic megacolon-a life-threatening swelling of the colon-happens in 2-4% of severe ulcerative colitis cases. These aren’t hypothetical risks. They’re real, documented outcomes.
The Diagnostic Divide: No Signs vs. Visible Damage
If you walk into a doctor’s office with bloating and diarrhea, how do they know if it’s IBS or IBD? They don’t guess. They test.
For IBD, they look for proof of damage:
- Colonoscopy with biopsy: Shows inflamed tissue, ulcers, crypt abscesses. 98% of confirmed IBD cases show these changes.
- Fecal calprotectin: A stool test that detects white blood cells in the gut. Levels above 250 µg/g mean active inflammation. IBS patients? Normal-under 50 µg/g.
- C-reactive protein (CRP): A blood marker for systemic inflammation. Over 5 mg/L? Likely IBD. Normal? Probably not.
- MRI or CT enterography: Shows thickened bowel walls, fistulas, abscesses-things IBS can’t cause.
For IBS? They do the opposite. They rule everything else out. If your blood work is clean, your stool tests show no infection or blood, your colon looks normal, and you don’t have weight loss or fever-then, and only then, do they say: “This is IBS.”
The CDC says it plainly: “Anemia, bleeding, weight loss, and fever are symptoms of IBD, not IBS. If you’re experiencing these, seek immediate medical treatment.”
Key Symptoms That Separate Them
Both can cause cramps, diarrhea, constipation, gas. But only one has these:
- Bloody stool: Common in IBD. Never normal in IBS.
- Black, tarry stools: Sign of upper GI bleeding-only seen in IBD.
- Unexplained weight loss: Happens in 65% of IBD flares. Rare in IBS.
- Fever: Present in 40% of moderate-to-severe IBD. Never in IBS.
- Joint pain, eye redness, skin rashes: These “extraintestinal” symptoms occur in 20-30% of IBD patients. IBS? No connection.
If you have blood in your stool, you don’t wait to see if it goes away. You go to the doctor. Now. That’s not a symptom of stress. That’s a sign your gut is being eaten from the inside.
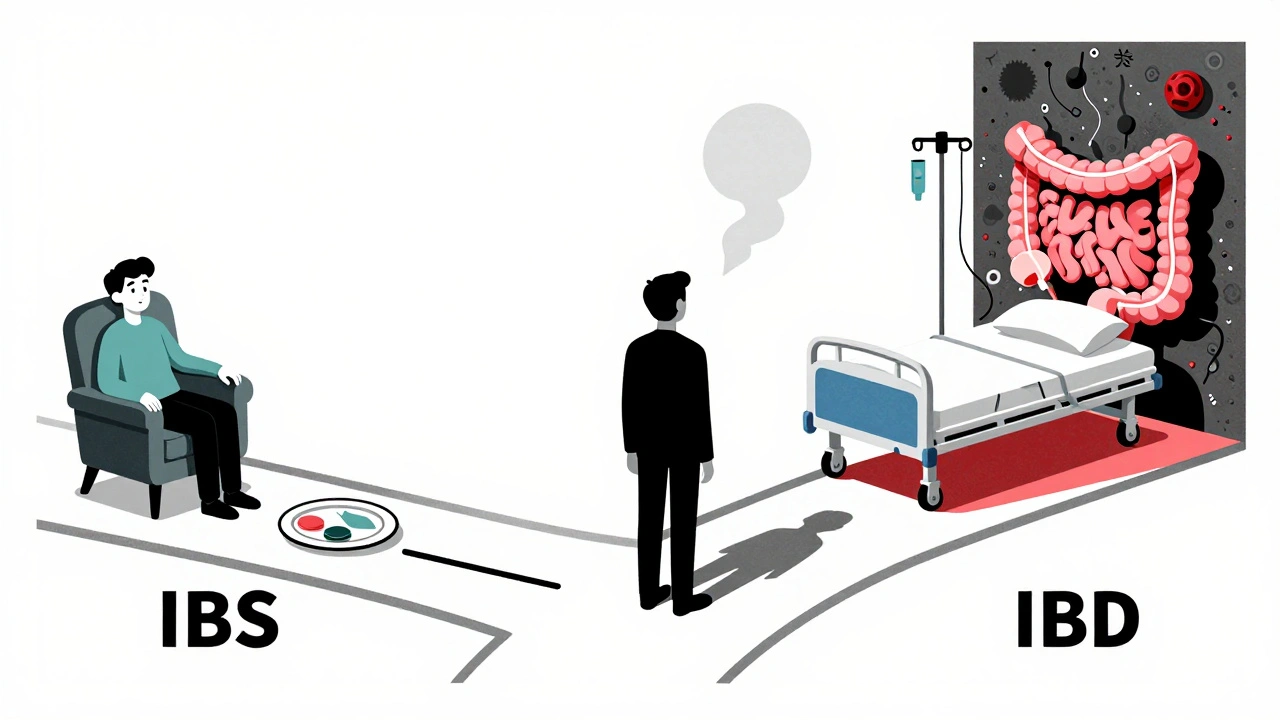
Treatment: Fixing the System vs. Fighting the Fire
IBS treatment is about calming the nervous system and avoiding triggers. IBD treatment is about stopping your immune system from destroying your body.
For IBS:
- Low-FODMAP diet: Reduces symptoms in 76% of people. It’s not magic-it’s removing fermentable carbs that fuel gas and bloating.
- Low-dose antidepressants: Not for depression. These drugs (like amitriptyline) calm nerve signals in the gut. They cut pain by 50% in 60% of IBS patients.
- Eluxadoline or linaclotide: Targeted meds for diarrhea or constipation. They don’t cure IBS-they help you live with it.
For IBD:
- Biologics (infliximab, vedolizumab): These drugs block specific immune signals. Infliximab puts 50-60% of Crohn’s patients into remission within 14 weeks.
- Corticosteroids: Powerful but short-term. They reduce inflammation fast-but cause bone loss, diabetes, and mood swings if used too long.
- Immunomodulators (azathioprine, methotrexate): Suppress the immune system long-term to prevent flares.
- Surgery: May be needed for strictures, fistulas, or cancer risk. Up to 33% of Crohn’s patients need bowel resection within 10 years.
There’s no pill to cure IBS. But there are ways to live well. There’s no cure for IBD either-but with the right drugs, many people never have another flare.
Can You Have Both?
Yes. And it’s more common than you think.
Studies show 22-35% of people with IBD in remission still meet the diagnostic criteria for IBS. Their inflammation is under control, but their gut nerves are still hypersensitive. That’s why some IBD patients keep having bloating, urgency, or pain-even when their colon looks perfect on a scope.
It’s not “all in your head.” It’s a layered problem: physical damage + nervous system dysfunction. Treating just one part isn’t enough.
Myth Busting: What Doctors Want You to Know
Myth: “IBS turns into IBD.”
Truth: It doesn’t. Not ever. The Crohn’s & Colitis Foundation says this outright: “IBS does not develop into IBD.”
Myth: “Stress causes IBS.”
Truth: Stress doesn’t cause it-but it makes it worse. The gut-brain connection is real. But IBS has biological roots: altered gut motility, increased pain sensitivity, and changes in gut bacteria.
Myth: “IBD is just a worse case of IBS.”
Truth: No. IBD is a different disease entirely. It’s not a progression. It’s a different mechanism. One is a wiring issue. The other is an autoimmune war.
Myth: “If my colonoscopy is normal, I don’t have IBD.”
Truth: Not always. Crohn’s can affect the small intestine, which a standard colonoscopy doesn’t reach. MRI or capsule endoscopy might be needed.
When to See a Doctor-Right Now
If you have any of these, don’t wait:
- Blood in your stool
- Unexplained weight loss
- Constant fever
- Severe abdominal pain that doesn’t improve
- Joint pain, red eyes, or skin rashes with gut symptoms
These aren’t signs of a bad diet or stress. They’re signs your body is under attack.
And if you’ve been told you have IBS-but you’re still losing weight or bleeding-get a second opinion. You might have IBD.
IBS is frustrating. IBD is dangerous. Both are real. But they demand different answers.
Can IBS turn into IBD?
No. IBS does not progress into IBD. They are completely different conditions. IBS is a functional disorder with no structural damage, while IBD involves chronic inflammation and tissue destruction. The Crohn’s & Colitis Foundation confirms there is no known pathway from IBS to IBD.
Is IBD an autoimmune disease?
Yes. IBD, including Crohn’s disease and ulcerative colitis, is classified as an autoimmune condition. The immune system mistakenly attacks the lining of the digestive tract, causing inflammation, ulcers, and scarring. This is different from IBS, which is not autoimmune and does not involve immune system attacks on the gut.
Can a colonoscopy rule out IBD?
A colonoscopy can detect ulcerative colitis and Crohn’s disease affecting the colon-but not always. Crohn’s can occur in the small intestine, which a standard colonoscopy doesn’t reach. If symptoms persist despite a normal colonoscopy, doctors may order MRI enterography, capsule endoscopy, or blood/stool tests to check for inflammation.
Do I need to take medication for life if I have IBS?
Not necessarily. Many people manage IBS with diet changes, stress reduction, and occasional medication. The low-FODMAP diet helps 76% of patients. Some use gut-directed therapies like low-dose antidepressants or antispasmodics only during flares. Unlike IBD, IBS doesn’t require long-term immunosuppressants or biologics.
Can IBD be cured?
There is no cure for IBD, but it can be put into long-term remission. Biologics, immunomodulators, and lifestyle changes can stop inflammation and prevent complications for years. Some people with ulcerative colitis may be cured by removing the colon, but this is major surgery and not always chosen. The goal is control, not cure.
Why do I have IBS symptoms even though my IBD is in remission?
It’s common. Up to 35% of IBD patients in remission still meet the criteria for IBS. When inflammation is controlled, the gut nerves can remain overly sensitive, causing bloating, urgency, and pain. This is called “post-inflammatory IBS.” It’s not a relapse of IBD-it’s a lingering functional issue that needs separate management.