Stopping a medication isn’t as simple as just skipping a pill. For many people, suddenly stopping drugs like antidepressants, opioids, or benzodiazepines can lead to intense withdrawal symptoms-sometimes dangerous ones. Medication tapering is the safe, gradual way to reduce your dose, but it only works if you and your provider are on the same page. Too often, patients feel blindsided when their doctor says, "We need to stop this." Others are told to cut back too fast, then left alone with anxiety, insomnia, or even seizures. The truth? Safe tapering isn’t just about the numbers on a prescription. It’s about communication, trust, and a plan made together.
Why Tapering Matters More Than You Think
Not all medications need to be tapered. But for drugs that affect your brain chemistry-like SSRIs, benzodiazepines, or opioids-the body adapts. Over time, it starts to rely on the drug to function normally. When you remove it too quickly, your nervous system goes into overdrive. That’s not "just side effects." That’s withdrawal.
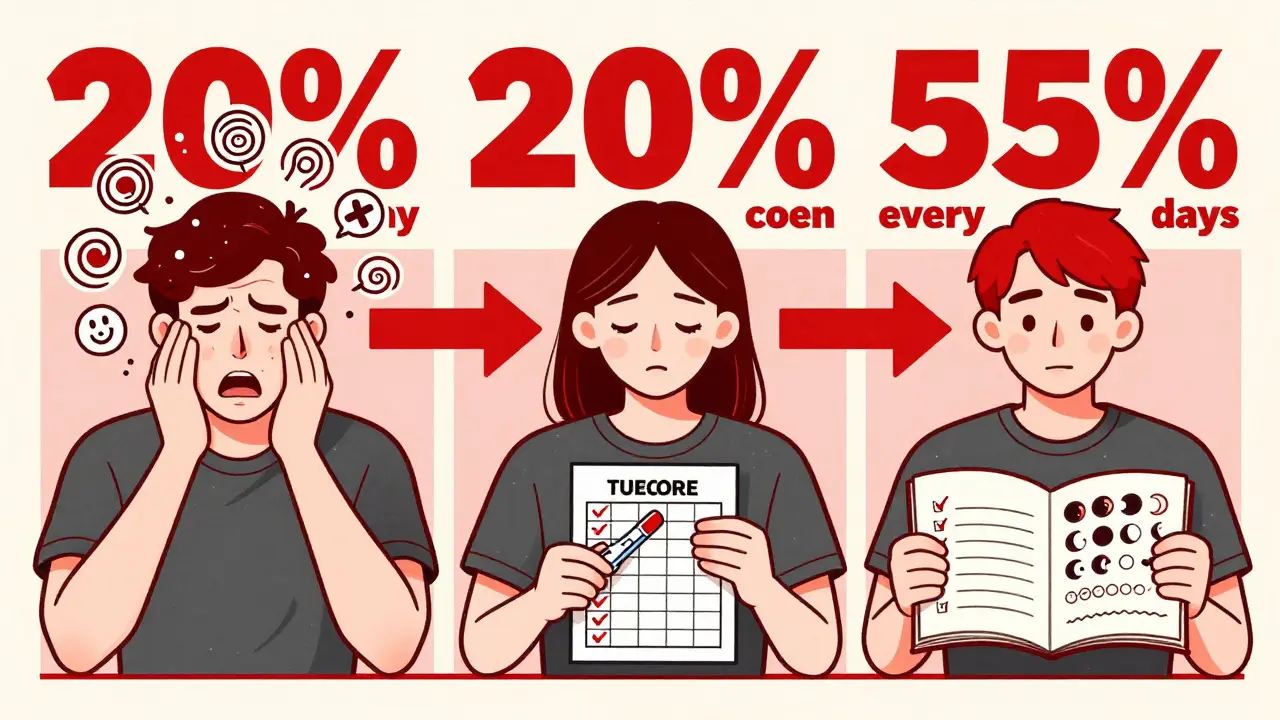
Studies show that 8-12% of long-term benzodiazepine users experience severe withdrawal, including panic attacks, muscle spasms, and seizures. Opioid tapering gone wrong can trigger intense pain, nausea, and even increase suicide risk. A 2021 JAMA study of 15,000 patients found that those who stopped opioids abruptly had 37% more emergency room visits than those who tapered slowly. And for antidepressants? A 2021 review found that 71% of clinical guidelines recommend tapering-but only 43% of doctors actually follow it.
The problem isn’t that doctors don’t know how. It’s that they don’t always talk about it. A 2023 survey of primary care clinics showed that only 41% of providers consistently involve patients in creating the taper plan. That’s not partnership. That’s instruction.
What Your Doctor Should Explain Before You Start
Before you even think about cutting your dose, your provider should walk you through five key things:
- Why this medication is being tapered. Is it because you’re feeling better? Because side effects are worse than the condition? Because long-term use carries risks? Be specific. If they say, "It’s just policy," ask for your personal reason.
- How long it will take. Tapering isn’t one-size-fits-all. A short-term user of a benzodiazepine might taper in 4 weeks. Someone on high-dose opioids for 5 years might need 6 months. The American Society of Addiction Medicine recommends reducing by 5-10% every 1-2 weeks for long-term users. Faster than that? You’re at higher risk.
- What symptoms to expect. Withdrawal isn’t just physical. It’s emotional. Anxiety, brain zaps, sleep disruption, and mood swings are common. Knowing what’s normal and what’s not helps you stay calm instead of panicking.
- How you’ll monitor progress. Will you keep a daily journal? Use an app? Have weekly check-ins? The best plans include clear signs for when to pause or slow down.
- What to do if things get worse. Who do you call? What’s the emergency plan? Can you get a temporary refill if symptoms flare? This isn’t optional. It’s essential.
One patient on Reddit shared: "My doctor said, ‘Just cut it in half.’ I had panic attacks for three weeks. I felt like I’d been lied to." That’s not a medical decision. That’s negligence.
How to Ask the Right Questions
If your provider brings up tapering, don’t just nod. Ask these questions:
- "Is this taper based on my health goals-or just because I’ve been on this too long?"
- "What’s the evidence for the schedule you’re suggesting?"
- "Can we try a slower pace first? I’d rather take longer than risk feeling awful."
- "Will I have access to support if symptoms get bad?"
- "Can I get a written plan with dates and dose changes?"
These aren’t challenging questions. They’re smart ones. The Centers for Disease Control and Prevention says tapering decisions must consider your functional status-not just your dose. If you’re stable, working, sleeping well, and not in pain, why rush? A 2021 study from the University of Washington found that mandatory rapid tapers for stable chronic pain patients led to a 60% increase in suicide attempts.
Different Medications, Different Rules
Not all drugs are the same. Your taper plan should match your medication.
| Medication Type | Typical Taper Duration | Reduction Schedule | Key Considerations |
|---|---|---|---|
| Benzodiazepines | 4-26 weeks | 5-10% every 1-2 weeks | Long half-life drugs like diazepam are easier to taper than short-acting ones like alprazolam. Switching to a longer-acting version first is often recommended. |
| Opioids | 2-6 months | 10% of original dose every 5-7 days | For high-dose users, the Department of Veterans Affairs recommends slowing down after reaching 30% of the original dose. Symptom management with clonidine or gabapentin may be needed. |
| Antidepressants (SSRIs) | 2-8 weeks | Varies widely: fluoxetine can be faster; paroxetine needs slow taper | Fluoxetine (Prozac) has a long half-life and may not need a taper. Paroxetine (Paxil) and venlafaxine (Effexor) are notorious for withdrawal. Some patients use specialized pill-cutting strips for micro-dose reductions. |
The Mayo Clinic reports an 85% success rate when following their 10% weekly taper method. But when patients were forced to cut by 20-50% per week, withdrawal symptoms jumped by 40-60%. Speed isn’t efficiency. It’s risk.
What Success Looks Like-From Real Patients
Patients who succeed at tapering have one thing in common: they were part of the plan.
- One woman on antidepressants said her doctor gave her a printed schedule with daily dose amounts, a symptom tracker, and a direct phone line. She completed the taper with no major issues.
- A man on long-term opioids asked for a 3-month plan instead of the 6-week one offered. His provider agreed. He reduced by 5% every 10 days. He felt in control. He didn’t relapse.
- A 2022 survey by the Mind charity found that 74% of people wanted more information about how long withdrawal would last. When providers gave clear timelines, anxiety dropped by 52%.
On the flip side, patients who felt rushed or ignored were far more likely to go back to their original dose-or worse, seek help in the ER.

Your Role in the Process
You’re not a passive recipient of a prescription. You’re a partner in your care. Here’s how to own your taper:
- Keep a daily log: note mood, sleep, energy, and any physical symptoms.
- Don’t wait until you’re in crisis to speak up. Say something at the first sign of trouble.
- Ask for a written plan. Email it to yourself. Print it. Keep it visible.
- Use a pill cutter or pharmacy compounding service if you need precise reductions.
- Know your limits. If your provider refuses to adjust the plan when you’re struggling, it’s okay to ask for a second opinion.
Remember: a good taper doesn’t feel like punishment. It feels like a roadmap. And you should never feel alone on the journey.
The Future of Safe Tapering
Change is coming. In 2023, the FDA required all long-acting opioid labels to include tapering instructions. Medicare now penalizes clinics with high ER visits after medication discontinuation. The American Society of Addiction Medicine launched an AI-powered tapering toolkit in early 2024 that generates personalized schedules based on your health history.
Next up? Pharmacogenomic testing. Clinical trials are underway to see if your genes can predict how you’ll respond to tapering. That means someday, your doctor might say, "Based on your CYP450 profile, we’ll reduce by 7% every 9 days."
But none of that matters if communication doesn’t improve. The biggest barrier to safe tapering isn’t lack of science. It’s lack of conversation.
Can I stop my medication cold turkey?
For some medications-like certain antibiotics or short-term pain relievers-yes. But for antidepressants, benzodiazepines, opioids, and other central nervous system drugs, stopping suddenly can be dangerous. Withdrawal symptoms can include seizures, severe anxiety, heart palpitations, and suicidal thoughts. Always talk to your provider before stopping.
How do I know if I need to taper?
If you’ve been taking a medication for more than 4-6 weeks, especially at daily doses, tapering is usually recommended. This includes SSRIs, SNRIs, benzodiazepines, opioids, and even some sleep aids. Your provider should review your usage, symptoms, and goals before deciding. Don’t assume you’re fine just because you feel okay-your body may have adapted without you realizing it.
What if my doctor won’t help me taper?
You have the right to safe, informed care. If your provider refuses to create a taper plan, ask for a referral to a pain specialist, psychiatrist, or addiction medicine provider. Many clinics now specialize in medication discontinuation. You can also contact organizations like the American Society of Addiction Medicine or Mind for provider directories. Don’t accept silence as an answer.
How long does withdrawal last?
It varies. For most people, acute withdrawal lasts 1-4 weeks. But some, especially with antidepressants or benzodiazepines, experience protracted symptoms-like brain zaps or low mood-for months. That doesn’t mean you’re failing. It means your nervous system is healing. Patience and support are key. If symptoms last longer than 3 months, talk to your provider about possible underlying issues.
Are there tools to help me taper at home?
Yes. Pharmacies can compound medications into precise doses. Pill cutters, digital trackers (like the ASAM Taper Toolkit), and symptom journals help you stay on track. Some apps even send reminders and allow you to share progress with your provider. But tools don’t replace communication. Use them alongside regular check-ins with your care team.
Final Thought: This Is Your Health
Medication isn’t just chemistry. It’s your life-your sleep, your mood, your ability to show up for work, family, or yourself. Tapering isn’t about quitting. It’s about reclaiming control. And the only way to do that safely is to talk-clearly, honestly, and repeatedly-with the person who knows your body best.
