When your child is prescribed a liquid antibiotic, you’re not just getting a bottle of medicine-you’re getting a time-sensitive treatment that can lose its power if stored wrong. Many parents assume all liquid antibiotics need to go in the fridge. That’s not true. Some will break down faster if chilled. Others won’t work at all if left on the counter. Getting this right matters because liquid antibiotics that lose potency won’t clear the infection. The bacteria survive. The illness lingers. And worse, it can grow stronger.
Not All Liquid Antibiotics Need the Fridge
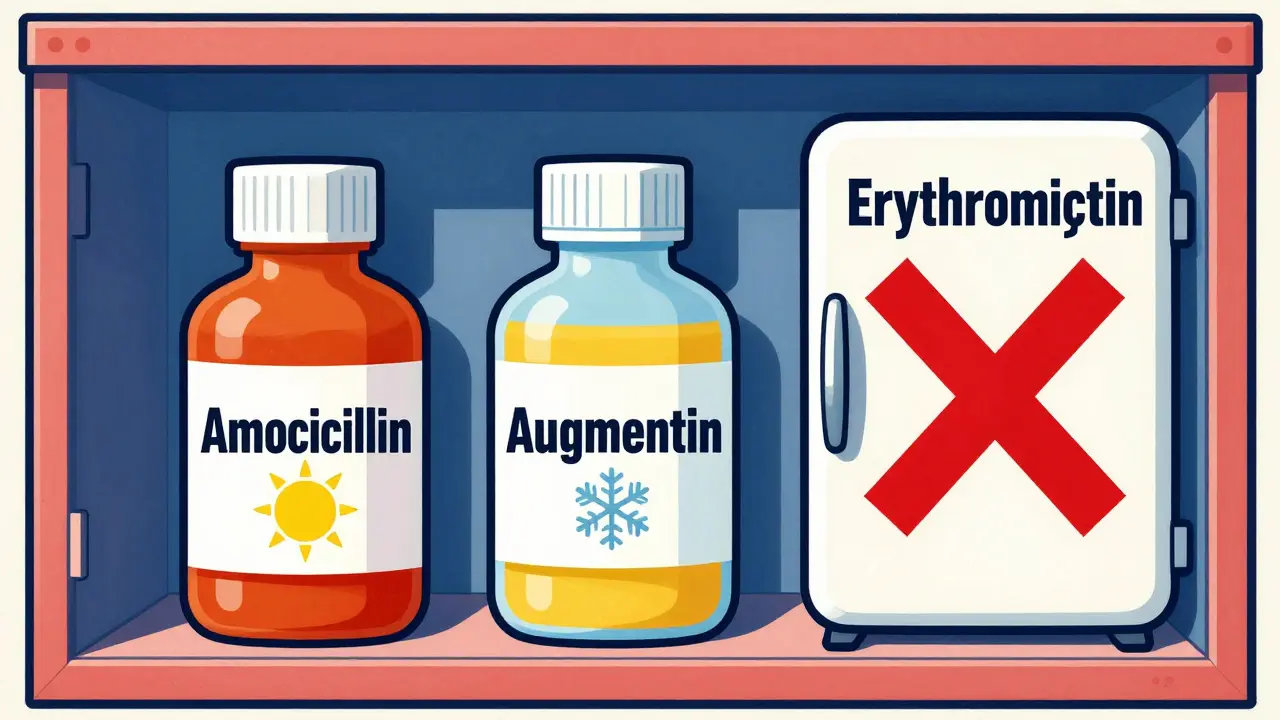
The biggest mistake people make? Assuming refrigeration is always better. It’s not. The FDA requires manufacturers to test each antibiotic suspension under real-world conditions before it hits the shelf. That means the storage instructions on the label aren’t suggestions-they’re science-backed requirements. For example, amoxicillin suspension can be stored at room temperature (68-77°F) for up to 14 days after mixing. Refrigeration helps it last longer and tastes better, but it’s not required. On the other hand, amoxicillin-clavulanate (Augmentin) is more sensitive. While some sources say it’s okay at room temperature for 10 days, others recommend refrigeration and strict 10-day discard rules. Why the difference? Because clavulanate, the second ingredient, breaks down faster than amoxicillin when it’s warm. So even if the liquid looks fine, it might not be strong enough to kill the bacteria. Some antibiotics, like certain cephalosporins or erythromycin suspensions, actually degrade faster in the cold. Refrigerating them can cause the active ingredients to separate or crystallize, making the dose uneven. That’s why Walgreens pharmacists warn: “Refrigerating certain liquid antibiotics will actually break down some medication, making them less effective.” Always check the label. If it doesn’t say “refrigerate,” don’t assume you should.Temperature Rules That Actually Matter
The ideal storage range for most medicines is between 59°F and 77°F-cool, dry, and away from sunlight. That’s the same as a typical closet or cabinet in your home. But here’s where people mess up:- Don’t store antibiotics on the windowsill. Sunlight breaks down chemicals. A bottle left in direct sun for a few hours can lose potency.
- Don’t leave them in the car. Even in winter, a car can drop below freezing. Antibiotics aren’t like juice-they don’t bounce back after freezing. Proteins and suspensions can permanently change structure.
- Don’t keep them in the bathroom. Humidity from showers ruins most pills and liquids. Moisture causes clumping, chemical breakdown, and mold.
How Long Do Reconstituted Antibiotics Last?
The expiration date on the bottle is for the powder before you mix it. Once you add water, the clock starts ticking. Here’s what the data shows:| Antibiotic | Refrigerated (2-8°C) | Room Temperature (20-25°C) | Discard After |
|---|---|---|---|
| Amoxicillin | Up to 14 days | Up to 14 days | 14 days |
| Amoxicillin-Clavulanate (Augmentin) | Up to 10 days | Up to 5 days | 5-10 days |
| Cephalexin | Up to 14 days | Up to 14 days | 14 days |
| Erythromycin | Not recommended | Up to 14 days | 14 days |
| Clindamycin | Up to 14 days | Up to 14 days | 14 days |

How to Measure Doses Correctly
A broken dose is just as dangerous as a spoiled one. Using a kitchen spoon? Don’t. A teaspoon varies by brand. A tablespoon can be off by 20%. That’s why the Cleveland Clinic says: “Use a specially marked oral syringe, spoon, or dropper.” These are calibrated to deliver exact amounts. Always shake the bottle well before each use. Suspensions settle. If you don’t shake, you might give your child a dose with no medicine at all-or too much. If the medicine has been sitting for more than a few hours, shake for 10-15 seconds. If it looks clumpy, gritty, or smells sour, throw it out. Don’t risk it.What Happens When You Store Antibiotics Wrong?
Improper storage doesn’t just mean “it won’t work.” It means the infection might not go away. And when that happens, the bacteria are still alive-and they’re being exposed to a weak dose of antibiotics. That’s how resistant strains form. Baystate Health reports that 30% of households store medications incorrectly. In rural areas with unreliable power, that number is even higher. Kiyingi and Lauwo’s 1993 study showed that in places without consistent refrigeration, antibiotics often lost potency before the end of the treatment course. That’s not just a waste of money-it’s a public health risk. The FDA warns that expiration dates assume proper storage. If your medicine sat in a hot car for two hours, it might be useless-even if it’s still within the printed expiration date. That’s why they require manufacturers to test stability under real conditions. But once it leaves the pharmacy, the chain breaks.
What to Do With Expired or Unused Liquid Antibiotics
Never flush them down the toilet or throw them in the trash. That pollutes water and puts them in reach of kids or pets. Instead:- Check if your pharmacy has a take-back program. Most do.
- Use a drug disposal kiosk at a local police station or hospital.
- If nothing’s available, mix the liquid with kitty litter, coffee grounds, or dirt. Pour it into a sealed container. Throw it in the trash.
Pro Tips for Real-Life Situations
- If your power goes out and the fridge warms up, assume the antibiotic is compromised. Call your pharmacist. Don’t guess.
- If you’re traveling and can’t refrigerate, ask your doctor if there’s a tablet version available. It’s often more stable.
- Write the date and time you mixed the antibiotic on the bottle. Use a permanent marker.
- Keep all medications out of reach of children-even if they taste sweet. Many liquid antibiotics are flavored to make them palatable, which makes them dangerous if found.
Antibiotics are powerful. But they’re not magic. They need to be handled right to work. Get the storage right, and you’re giving your child the best chance to get well-fast.
Do all liquid antibiotics need to be refrigerated?
No. Some, like amoxicillin, can be stored at room temperature (68-77°F) for up to 14 days. Others, like amoxicillin-clavulanate, are more stable when refrigerated. Some, like erythromycin, can actually break down faster in the fridge. Always check the label or ask your pharmacist.
How long can I keep reconstituted amoxicillin?
Amoxicillin suspension can be kept at room temperature or in the refrigerator for up to 14 days after mixing. After that, even if it looks fine, throw it away. The potency drops over time, and you won’t know how much is left.
Can I freeze liquid antibiotics to make them last longer?
Never freeze liquid antibiotics. Freezing can permanently damage the structure of the suspension, causing the active ingredients to separate or degrade. This makes the dose unpredictable and potentially ineffective. Always store at the temperature specified on the label.
What if my child didn’t finish the full course? Can I save the rest?
No. Even if there’s medicine left, don’t save it. Antibiotics are prescribed for a specific infection, dose, and duration. The leftover liquid may be expired, contaminated, or not strong enough for a new illness. Using it without a doctor’s approval can lead to antibiotic resistance or mask a more serious problem.
How do I know if my antibiotic has gone bad?
Signs include: clumps or particles that don’t shake out, unusual color changes, a sour or off smell, or separation that won’t mix back in. If you’re unsure, call your pharmacist. Never guess-using a degraded antibiotic can delay recovery and make infections harder to treat.
Can I use a regular kitchen spoon to measure the dose?
No. Kitchen spoons vary too much in size. A teaspoon can hold anywhere from 3 to 7 milliliters. That’s a dangerous margin of error. Always use the oral syringe, dropper, or dosing cup that came with the medicine. They’re calibrated for accuracy.