Every time you pick up a prescription, there’s a good chance the pharmacist handed you a generic version instead of the brand-name drug your doctor wrote on the script. That’s not a mistake-it’s the law. But here’s the catch: pharmacy substitution laws aren’t the same in every state. What’s allowed in California might be illegal in Oklahoma. If you’re switching states, moving to a new pharmacy, or just trying to save money on meds, understanding how these rules work in your area is critical.
What Exactly Is Pharmacy Substitution?
Pharmacy substitution means a pharmacist swaps a brand-name drug for a generic or biosimilar version without contacting your doctor first. This isn’t just about saving a few bucks-it’s a system designed to cut U.S. drug spending by billions. Generic drugs cost 80-85% less than their brand-name counterparts, according to the FDA. In 2023, generics made up 90% of all prescriptions filled in the U.S. but only 23% of total drug spending. That’s a $313 billion annual savings. But not all drugs are created equal. For most pills-like statins, blood pressure meds, or antibiotics-generics work just as well. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration. They’re tested to ensure they deliver the same effect in the body. Where things get tricky is with drugs that have a narrow therapeutic index (NTI). These are medications where even tiny differences in how the body absorbs the drug can cause serious side effects or make the treatment fail. Examples include warfarin (a blood thinner), phenytoin (for seizures), and levothyroxine (for thyroid issues). Some states ban substitution for these drugs entirely. Others allow it-but only with extra steps.How Your State Handles Substitution: Mandatory, Permissive, or Restrictive
All 50 states and Washington, D.C. have laws about when pharmacists can substitute. But they fall into three basic categories:- Mandatory substitution (19 states): The pharmacist must switch to a generic unless the doctor says not to. States like New York, California, and Texas use this model.
- Permissive substitution (31 states + D.C.): The pharmacist can substitute, but doesn’t have to. They have discretion. This is the most common setup.
- Restrictive (none officially): No state outright bans substitution, but some add heavy restrictions-for example, requiring prescriber approval for certain drugs.
Do You Have to Be Told About the Switch?
This is where patients get caught off guard. In 19 states, pharmacists aren’t required to tell you they substituted your drug. That means you could walk out with a different pill, different label, different color-and never know. But 31 states plus D.C. require some kind of notification. Some just send a paper notice with your prescription. Others require the pharmacist to verbally tell you at the counter. Seven states, including Massachusetts and New Jersey, require your explicit consent before substitution happens. That means they can’t swap your drug unless you say yes. For biologics-complex drugs like Humira, Enbrel, or insulin-the rules are even stricter. Only 10 biosimilars in the U.S. have received the FDA’s "interchangeable" designation, meaning they can be swapped like generics. But even then, 45 states require extra steps: notifying your doctor, waiting for approval, or proving the biosimilar costs less than the brand.
What Can You Do as a Patient?
You have rights-even if your state’s laws are vague. Here’s what you can do:- Ask for the generic at the pharmacy counter. Even in permissive states, pharmacists often default to the brand unless you ask. Say: "Is there a generic version of this? I’d like to save money if it’s safe."
- Check your prescription label. Generic drugs have different names. If you see "irbesartan" instead of "Avapro," that’s a substitution. If you don’t recognize the name, ask.
- Know your state’s rules. Visit your state board of pharmacy’s website. Search for "drug product selection law" or "generic substitution." You’ll find exact guidelines on what’s allowed.
- Request "dispense as written" on your prescription. Your doctor can write this on the script to block substitution. In 28 states, they have to give a reason why-so if you’re worried about safety, ask them to note "NTI drug" or "history of adverse reaction."
- Refuse substitution. You can say no-even if your state allows it. Pharmacists can’t force you to take a different drug. If they push back, ask to speak to the pharmacist-in-charge.
What Pharmacists Need to Know
If you’re a pharmacist-or work with one-this is your reality: you’re caught between cost-saving mandates and legal liability. In 24 states, there’s no clear protection from malpractice claims if a substituted drug causes harm, even if you followed the law. That’s why many pharmacists err on the side of caution. They’re also dealing with confusing labels. The FDA’s "biosimilar" and "interchangeable" designations aren’t always clear to patients-or even to pharmacists. A 2022 survey found 67% of pharmacists initially confused the two terms. Interchangeable biosimilars can be swapped automatically, like generics. Biosimilars that aren’t interchangeable require prescriber approval. Plus, 15 states prohibit substitution if the biosimilar costs more than the brand-even if your insurance covers the brand at $0 copay. That means a $500 biosimilar can’t replace a $450 brand-name drug, even if the brand is cheaper for you. It’s a mess.What’s Changing in 2025?
The landscape is shifting. California’s AB1881, effective in 2023, now requires pharmacists to give patients a written notice and verbal explanation for every biosimilar substitution. New York expanded substitution rights for certain biosimilars in early 2023. Florida, Georgia, and Illinois now require dual notification-both patient and prescriber must be informed within 24-72 hours. The National Association of Boards of Pharmacy is pushing for a model law to standardize rules across states. So far, 22 states have adopted parts of it-focusing on consistent documentation and notification timelines. By 2030, biosimilars could make up 70% of the U.S. biologics market. But that won’t happen unless states simplify their laws. Right now, a patient moving from Texas to Oregon might find their insulin suddenly switched-or denied-because of a paperwork gap.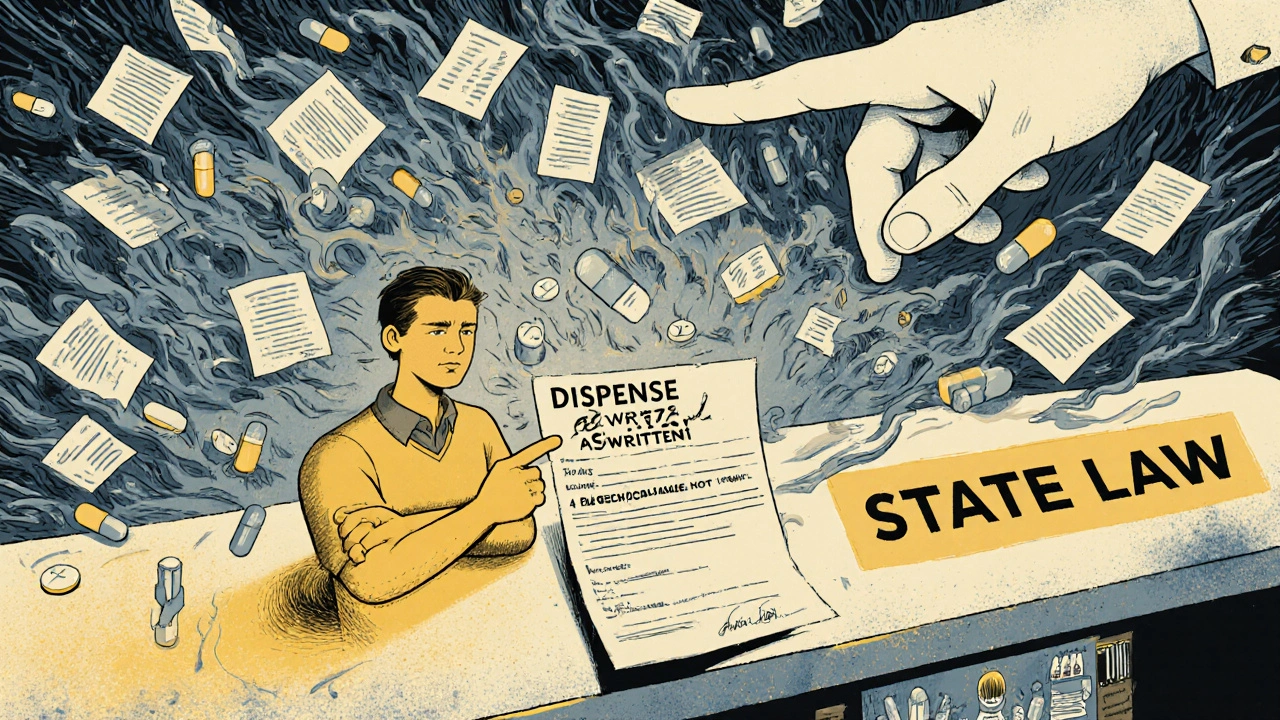
Real-Life Scenarios: What Could Go Wrong
A 68-year-old woman in Ohio gets her warfarin filled. The pharmacist substitutes a generic because Ohio allows it. She doesn’t notice the change. Two weeks later, she has a minor bleed. Her INR levels are off-not because the generic is bad, but because her body absorbed it slightly differently. She didn’t know to tell her doctor about the switch. A teenager in Alabama gets a biosimilar for psoriasis. His mom doesn’t know it’s not the same as the original drug. When his flare-ups return, he blames the medicine, not the substitution. He stops taking it. His condition worsens. These aren’t rare cases. They’re symptoms of a system that’s fragmented.Where to Find Your State’s Rules
Don’t guess. Don’t rely on your pharmacist’s memory. Go straight to the source:- Search: "[Your State] Board of Pharmacy generic substitution law"
- Look for the section on "Drug Product Selection" or "Pharmacist Substitution Authority."
- Check if your state has a "negative formulary"-a list of drugs that can’t be substituted. NTI drugs are usually on it.
- See if your state requires patient consent, notification, or prescriber alert.
Bottom Line: Know Your Rights, Know Your State
Generic drugs save money. Biosimilars will save even more. But without clear rules and clear communication, those savings come with risk. Whether you’re a patient, a caregiver, or a provider, the key is this: don’t assume substitution is automatic. Ask questions. Check your label. Know your state’s law. And if something feels off-speak up.It’s not just about cost. It’s about control. You deserve to know what’s in your body-and why.
Can my pharmacist substitute my brand-name drug without telling me?
In 19 states, yes-pharmacists aren’t legally required to notify you before substituting a generic drug. In 31 states plus D.C., they must provide some form of notification, either verbally, in writing, or on the label. Always check your prescription label for the drug name. If it’s different from what your doctor prescribed, ask why.
What’s the difference between a biosimilar and an interchangeable drug?
A biosimilar is a biologic drug that’s highly similar to the original, but not identical. An interchangeable biosimilar has been proven to produce the same clinical result as the original and can be substituted without the prescriber’s involvement-just like a generic. Only 10 biosimilars in the U.S. have interchangeable status as of late 2023. Most are not interchangeable, so substitution requires extra steps.
Can I refuse a generic or biosimilar substitution?
Yes. You can refuse any substitution in every state. Pharmacists must honor your request-even if the law allows substitution. If they pressure you or act surprised, ask to speak to the pharmacist-in-charge. Your right to choose your medication is protected under patient autonomy laws.
Why do some states ban substitution for certain drugs like warfarin or phenytoin?
These drugs have a narrow therapeutic index, meaning small differences in how your body absorbs them can lead to serious side effects or treatment failure. Studies show states with restrictions on substituting these drugs have 18% fewer adverse events. Even though generics are FDA-approved, the risk isn’t zero-so many states err on the side of caution.
How do I know if my state requires prescriber approval for biosimilar substitution?
Twelve states require prior authorization from your doctor before a biosimilar can be substituted. Others require notification within 24 to 72 hours. Check your state board of pharmacy’s website for their specific biosimilar substitution rules. Look for terms like "prior authorization," "physician notification," or "interchangeable product requirements."
Can my doctor prevent substitution even if my state allows it?
Yes. In every state, your doctor can write "dispense as written" or "do not substitute" on your prescription. In 18 states, they must also provide a reason-like "narrow therapeutic index" or "patient history of adverse reaction." This is your best tool if you’re concerned about switching.
