Storing medications safely in a shared home isn’t just a good idea-it’s a necessity. Whether you’re living with aging parents, adult children, roommates, or in an assisted living facility, the risk of accidental poisoning, misuse, or lost doses is real. In 2025, over 59 million U.S. households include multiple generations under one roof, according to the U.S. Census Bureau. That’s nearly one in four homes where someone’s pills could end up in the wrong hands-or the wrong stomach.
Why Medication Storage Matters More Than You Think
Medications aren’t candy. Even common over-the-counter drugs like ibuprofen or antihistamines can cause serious harm if taken by the wrong person. Children might grab what looks like a colorful tablet. Someone with memory issues might double-dose. Or worse, a roommate might take a painkiller meant for someone else because they’re in pain and don’t want to ask. The data doesn’t lie. A 2025 survey by SeniorHelpers found that 67% of multi-generational households had at least one medication-related incident in the past year. Nearly half of those involved kids pulling pills from bathroom cabinets or kitchen counters. In assisted living facilities, 13% of inspections between 2020 and 2021 found violations linked to improper storage, according to the Joint Commission. That’s not just a paperwork problem-it’s a safety crisis.Lock It Up. Every Time.
The simplest, most effective rule: medications must be locked away. No exceptions. In professional care settings, 100% of large facilities use locked medication carts or rooms. But in homes? Only 28% of families use locked storage, according to SeniorHelpers. That’s a dangerous gap. You don’t need a fancy safe. A simple lockbox with a key or combination works. Keep it out of sight-inside a bedroom closet, on a high shelf, or even bolted to the wall. Avoid bathroom cabinets. Humidity ruins pills. And kids know where the toothpaste is. Controlled substances like opioids, benzodiazepines, or ADHD meds? Those need a lock that only authorized people can open. Some smart locks now track who opens them and when. DosePacker released one in March 2024 that logs every access. It’s not cheap, but for high-risk meds, it’s worth it.Temperature Isn’t Optional
Not all meds can sit on a shelf. Insulin, some antibiotics, eye drops, and biologics need refrigeration. But your kitchen fridge isn’t a medicine cabinet. The center shelf of the fridge is the coldest, most stable spot. Door shelves swing 10°F or more every time you open the door. That’s enough to ruin insulin. A user on CareGiverForum shared that after storing her father’s insulin on the door for three weeks, his blood sugar went haywire. Turns out, the heat ruined it. Best practice: Use a dedicated mini-fridge just for meds. If that’s not possible, label the shelf clearly: “MEDICATIONS ONLY. DO NOT STORE FOOD HERE.” The FDA updated its guidance in February 2024 for 47 commonly prescribed drugs, including newer diabetes and MS treatments. Always check the label or ask your pharmacist. If it says “refrigerate,” treat it like milk-not a suggestion.Label Everything. Even the Obvious Stuff
You know what “MOM’S BP PILLS” means. But what if a grandkid finds it? Or a nurse comes to help? Or someone else in the house needs to give a dose? Every container should have:- The person’s full name
- The drug name and strength
- How often to take it
- Expiration date

Sort by Type and Need
Don’t just dump all meds into one box. Group them:- Regular daily meds (blood pressure, thyroid, etc.)
- As-needed meds (pain relievers, anxiety meds)
- Refrigerated items
- Over-the-counter drugs (even aspirin or allergy pills)
Document What You Have
In care homes, staff keep Individualized Medication Administration Records (MARs). That’s a daily log of who took what and when. Most families don’t do this. But you should. Start simple. Use a notebook or a free app like Medisafe or MyTherapy. Write down:- Medication name
- Dose
- Time taken
- Who gave it
- Any side effects
Get Rid of the Junk
Old pills gather dust. And danger. Every six months, do a full medication audit. Pull out everything: prescriptions, vitamins, leftover antibiotics, that cough syrup from 2021. Check expiration dates. If it’s expired, throw it out. If it’s a controlled substance, don’t just toss it. The FDA and DEA recommend using drug take-back programs. Many pharmacies, police stations, and hospitals have drop boxes. You can also mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. Never flush them unless the label says to. In one Oregon household, a teen found a bottle of old oxycodone in a drawer. He didn’t take it-but he showed it to his friends. That’s how addiction starts.Training and Communication
Everyone in the home needs to know the rules. In assisted living, staff get 8-12 hours of training and quarterly refreshers. In homes? No one gets trained. That’s a problem. Hold a 15-minute family meeting. Show everyone where the meds are kept. Explain why they’re locked. Tell kids: “This isn’t candy. If you touch it, we’ll have to move it to a place you can’t reach.” SeniorHelpers launched a free Medication Safety Certification for caregivers in April 2025. Over 12,500 people signed up in the first month. You can find it online-it takes 30 minutes. Worth it.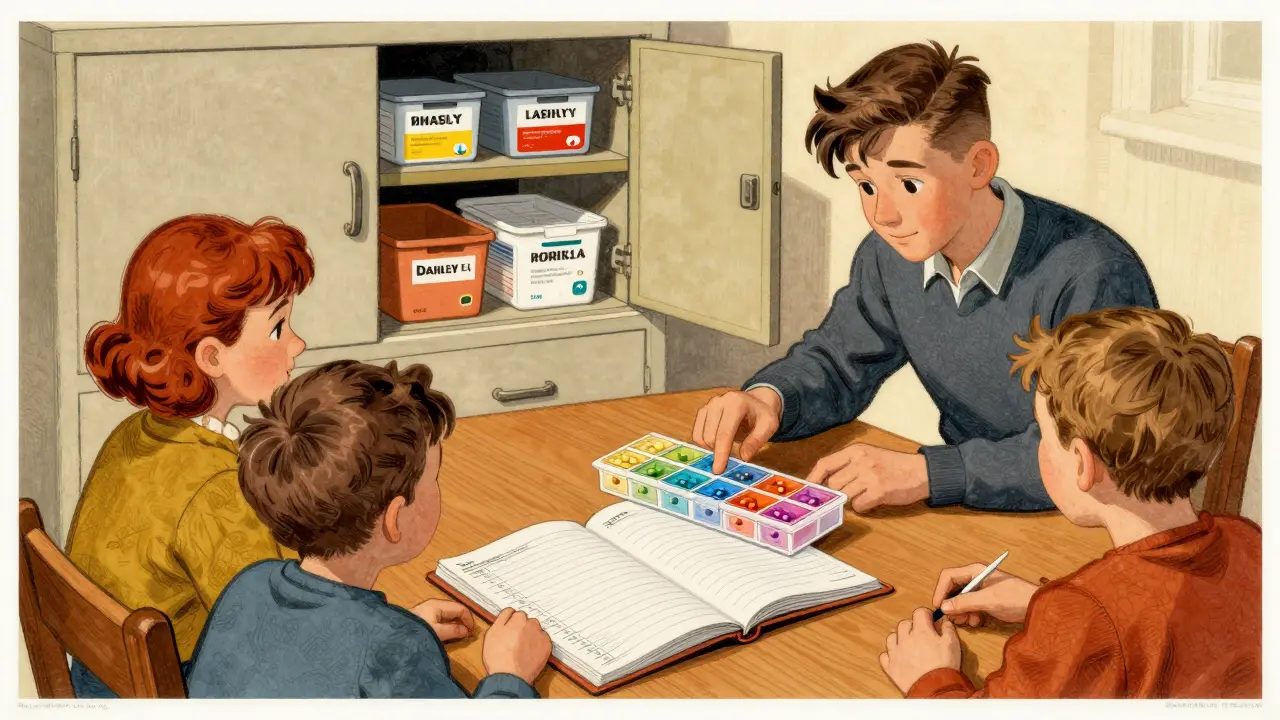
What About Shared Living Facilities?
If you’re in an assisted living home or group setting, ask these questions:- Are meds stored in a locked room or cart?
- Is there a dedicated fridge for refrigerated meds?
- Do staff log every dose given?
- Are temperature logs kept?
- Who has access to the key or code?
What’s New in 2026?
Tech is catching up. Smart medication cabinets now monitor temperature, humidity, and access. Some even alert staff if a dose is missed or if the door was left open. By 2027, over 65% of care facilities are expected to use these systems, up from just 22% in 2024. For homes, smart lockboxes with app alerts are dropping in price. You can now get one with a digital keypad and remote access for under $80. AI-powered systems are in testing at 15 facilities. Cameras watch the storage unit and flag if a pill bottle is opened at the wrong time. It’s not mainstream yet-but it’s coming.Final Checklist
Use this every three months:- ✅ All meds locked in a secure container
- ✅ Refrigerated items stored in the center of the fridge
- ✅ Each pill labeled with name, dose, and expiration
- ✅ Expired or unused meds properly disposed of
- ✅ Everyone in the home knows where meds are and why they’re locked
- ✅ A simple log (paper or app) tracks who takes what and when
Frequently Asked Questions
Can I store all my medications in one box?
You can, but you shouldn’t. Group them by type-daily meds, as-needed meds, refrigerated items, and OTC drugs. This reduces confusion and helps prevent mistakes. Use small bins or dividers inside your locked box to keep things organized.
Is it okay to keep meds in the bathroom?
No. Bathrooms are too humid and hot, especially near showers. Moisture can make pills lose strength or break down. Store meds in a cool, dry place like a bedroom drawer or closet. If you must use the bathroom, keep them in a sealed container away from the sink and shower.
What if someone in the house has a substance use disorder?
That changes everything. Controlled substances like opioids or benzodiazepines must be stored in a lockbox with limited access-ideally only one trusted person holds the key. Consider a smart lock that logs access. Talk to a pharmacist or social worker about additional safety steps. Never assume someone won’t take them. The risk is too high.
How do I dispose of old or expired meds safely?
Use a drug take-back program at a pharmacy or police station. If that’s not available, mix pills with cat litter or coffee grounds, seal them in a plastic bag, and throw them in the trash. Never flush them unless the label says to. For controlled substances, check with your local DEA office-they often have special disposal events.
Do I need to log every dose if I’m not a professional?
Yes. Even in a family home, a simple log helps prevent double-dosing or missed doses. Use a notebook, whiteboard, or free app like Medisafe. Write the name, time, and who gave it. It takes 30 seconds a day but can prevent a hospital visit.
What’s the best type of lockbox for home use?
A small, durable combination or key lockbox that fits on a shelf or mounts to the wall. Look for one with a tamper-proof design. Smart lockboxes with app alerts cost more but give you peace of mind-especially if you’re not home often. Brands like DosePacker and MedMinder offer models under $100.
