Hormonal Irritation Checker
How Hormone-Related Is Your Irritation?
Answer these questions to get personalized guidance on whether hormonal changes are likely causing your symptoms.
- Estrogen and progesterone levels directly affect vaginal moisture and pH, making irritation more likely during certain life stages.
- Menstrual cycle peaks, pregnancy, menopause, and hormonal birth control each have distinct irritation patterns.
- A simple symptom checklist can help you pinpoint whether hormones are the main driver.
- Non‑prescription moisturizers, probiotic gels, and lifestyle tweaks often relieve mild cases.
- Seek medical advice if irritation persists, is painful, or is accompanied by unusual discharge.
Vaginal irritation is frustrating, but you don’t have to guess what’s causing it. In many cases, the culprit is a shift in your body’s hormonal changes. Understanding how hormones like estrogen and progesterone interact with vaginal tissue can turn guesswork into a clear plan of action.
What is Vaginal Irritation?
When the delicate lining of the vagina becomes red, itchy, or painful, we call it vaginal irritation. It’s a symptom, not a disease, and can stem from infection, allergic reactions, or dryness. To separate hormone‑related irritation from other causes, we first need to know what the vagina normally looks like.
Vaginal irritation is a symptom characterized by itching, burning, redness, or discomfort in the vaginal area, often resulting from changes in moisture, pH, or tissue health. A healthy vagina stays moist, slightly acidic (pH 3.8‑4.5), and populated with beneficial bacteria called Lactobacilli.
How Hormones Influence Vaginal Tissue
Estrogen and progesterone are the primary players, but they don’t act alone. Each hormone shapes the vaginal environment in specific ways:
- Estrogen promotes the growth of the vaginal epithelium, increases blood flow, and boosts glycogen production, which feeds Lactobacilli. Higher estrogen means more moisture and a stable acidic pH.
- Progesterone tends to relax smooth muscle and can slightly raise vaginal pH, making the environment less hostile to harmful microbes. When progesterone dominates, some women notice mild dryness.
- Testosterone is present in low levels but contributes to local tissue elasticity and libido. Fluctuations can affect the sensation of irritation.
The balance of these hormones shifts throughout the menstrual cycle, during pregnancy, and when you enter menopause. Each phase brings a predictable pattern of irritation risk.
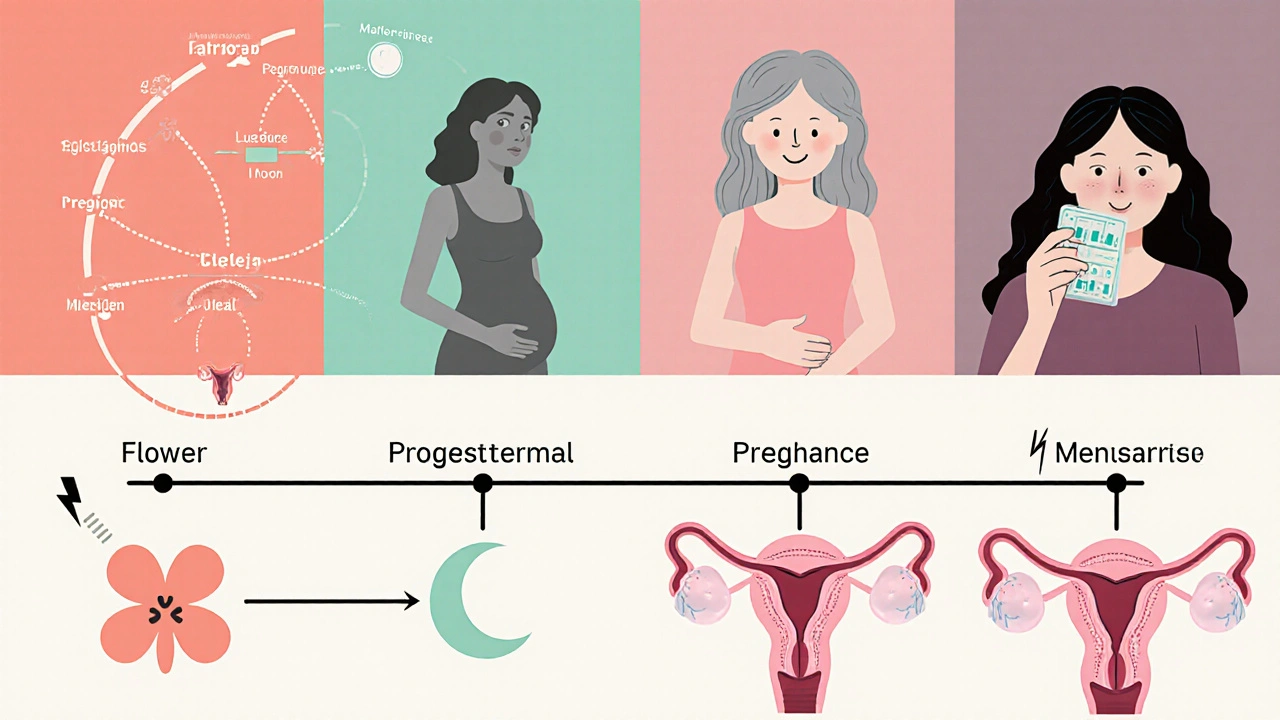
Life Stages Where Hormonal Shifts Trigger Irritation
Below is a quick rundown of the most common periods when hormonal swings make irritation more likely.
- Follicular phase (days 1‑14 of the cycle): Rising estrogen enhances lubrication, so irritation is usually low. However, a sudden surge can cause temporary itching for some women.
- Luteal phase (days 15‑28): Progesterone peaks, and some women report mild dryness or a “tight” feeling.
- Pregnancy: Estrogen skyrockets (up to 30‑fold), boosting blood flow but also increasing sensitivity. Many pregnant women experience itching due to stretched skin and hormonal “over‑lubrication.”
- Menopause: Estrogen drops dramatically, leading to atrophic vaginitis-thin, dry, and fragile tissue that burns or aches.
- Hormonal birth control: Pills, patches, or hormonal IUDs manipulate estrogen/progesterone ratios. Some users notice reduced irritation; others develop dryness, depending on the formulation.
Common Irritation Symptoms Linked to Hormones
Knowing the symptom‑to‑hormone connection helps you decide when to treat at home versus when to see a clinician.
| Hormone Change | Typical pH Shift | Common Symptoms |
|---|---|---|
| Estrogen ↑ (mid‑cycle, pregnancy) | pH stays ≤4.5 (acidic) | Increased moisture, occasional itching from over‑sensitivity |
| Progesterone ↑ (luteal phase, some contraceptives) | pH may rise to 4.5‑5.0 | Dryness, mild burning, feeling of tightness |
| Estrogen ↓ (menopause, post‑birth control cessation) | pH often >5.0 (less acidic) | Dryness, itching, burning, soreness, occasional bleeding |
Quick Checklist: Is Hormone‑Driven Irritation Likely?
- Are symptoms timed with a specific phase of your cycle or a life stage (pregnancy, menopause)?
- Do you use hormonal birth control, and did symptoms start after a formulation change?
- Is the discharge thin, clear, and non‑foul smelling (often hormone‑related) versus thick, fishy (suggests infection)?
- Have you noticed changes in vaginal pH or dryness after a recent health event (e.g., surgery, chemotherapy)?
- Do over‑the‑counter moisturizers or lubricants provide temporary relief?
If you answered “yes” to most of these, hormones are probably playing a big role.
Managing Hormone‑Related Vaginal Irritation
Below are practical steps you can try before scheduling a doctor’s visit.
- Hydrate and Eat Well: Staying hydrated helps maintain natural lubrication. Foods rich in phytoestrogens (soy, flaxseed) may subtly support estrogen levels during menopause.
- Use Water‑Based Lubricants: Look for glycerin‑free formulas to avoid yeast overgrowth.
- Apply Vaginal Moisturizers: Products containing hyaluronic acid or natural oils (e.g., coconut oil) can replenish moisture for weeks.
- Consider Probiotic Supplements: Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14 have shown modest benefits in restoring vaginal flora.
- Review Birth Control Options: If a pill is causing dryness, talk to your provider about switching to a lower‑dose formulation or a non‑hormonal IUD.
- Hormone Therapy for Menopause: Low‑dose estrogen creams or tablets can dramatically improve atrophic symptoms. Must be prescribed after a risk assessment.
- Avoid Irritants: Fragranced soaps, douches, and tight synthetic underwear can exacerbate dryness.
These measures target the hormonal root cause while also soothing the surface irritation.

When to Seek Professional Help
Self‑care works for mild, predictable irritation, but certain red flags warrant a medical exam:
- Severe burning or pain that interferes with daily activities.
- Bleeding outside of menstrual periods.
- Discharge that is thick, yellow, green, or has a strong odor (possible infection).
- Sudden onset after starting a new medication or hygiene product.
- Persistent symptoms for more than two weeks despite home treatment.
A clinician can run a wet‑prep, pH test, or hormone panel to rule out infections, atrophic changes, or endocrine disorders like PCOS.
Frequently Asked Questions
Can low estrogen during menopause cause yeast infections?
Low estrogen reduces glycogen, which feeds Lactobacilli. When good bacteria decline, Candida can overgrow, leading to yeast infections. Moisturizing and probiotic strategies help, but a doctor may prescribe antifungals if needed.
Why does my birth control pill make my vagina feel dry?
Combined oral contraceptives contain estrogen and progestin. Some formulations bias toward progestin, which can reduce vaginal secretions. Switching to a pill with higher estrogen or a non‑hormonal method often restores moisture.
Are over‑the‑counter lubricants safe during pregnancy?
Yes, most water‑based, glycerin‑free lubricants are pregnancy‑safe. Avoid those with parabens or fragrances, as they can irritate sensitive tissue.
How can I test my vaginal pH at home?
pH test strips (available at pharmacies) are simple: insert a strip into the vaginal wall for a few seconds, compare the color change to the chart. Normal is 3.8‑4.5; higher values suggest imbalance.
Is there a diet that supports vaginal health?
A diet rich in prebiotic fibers (e.g., garlic, onions, bananas) feeds Lactobacilli. Adding fermented foods like yogurt or kefir introduces live cultures. Limiting sugar helps keep yeast growth in check.
Next Steps
If you suspect hormones are behind your irritation, start with the checklist and self‑care tips above. Track symptoms in a calendar to see if they line up with your cycle or life changes. When in doubt, schedule a visit with a gynecologist-especially if any red‑flag signs appear.
Understanding the role of hormonal changes refer to fluctuations in estrogen, progesterone, and other endocrine factors that affect bodily functions, including the health of the vaginal mucosa. empowers you to make smarter choices and get relief faster.