Antibiotic Treatment Comparison Tool
Select infection type and condition to view treatment options
Antibiotics are medicines that kill or stop the growth of bacteria. They have saved millions of lives since the mid‑20th century, but they’re not a one‑size‑fits‑all solution. When it comes to infections of the gut or the vagina, the right drug, dose, and timing matter a lot.
Why a Separate Look at Intestinal and Vaginal Infections?
Both the gut and the vagina host complex communities of microbes that keep us healthy. Disrupt those communities, and you can get an infection. Yet the bacteria that cause trouble in each area are often different, and the way antibiotics interact with the local environment also varies. That’s why doctors treat them separately.
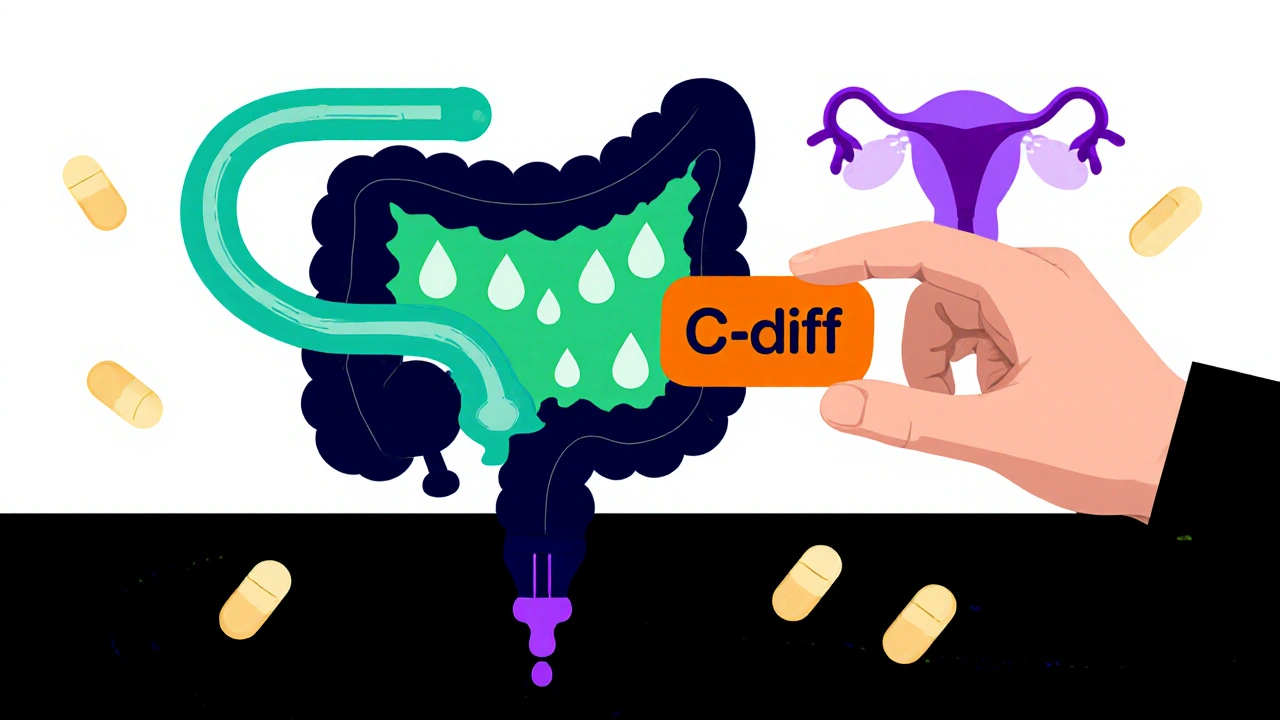
Common Bacterial Culprits
Intestinal infection can be caused by Clostridioides difficile (often just C. diff), Salmonella, or Campylobacter. In the vagina, the most frequent bacterial troublemakers are Bacterial vaginosis‑associated anaerobes and, less commonly, Streptococcus species.
How Antibiotics Work in the Gut
In the intestines, antibiotics must survive stomach acid and reach the colon where many pathogens live. Drugs like metronidazole, vancomycin, or fidaxomicin are chosen because they stay active in the anaerobic (low‑oxygen) environment of the colon. For example, metronidazole penetrates the gut wall, disrupts bacterial DNA, and is especially good against C. diff.
- Metronidazole - works on anaerobes, taken orally 500 mg three times daily.
- Vancomycin - given orally (not IV) for severe C. diff, 125 mg four times a day.
- Fidaxomicin - a newer option, 200 mg twice daily, with lower recurrence rates.
Because antibiotics also hit the good bacteria, many patients experience diarrhea or yeast overgrowth after treatment. Adding probiotics like Lactobacillus rhamnosus GG can help restore balance.
How Antibiotics Work in the Vagina
The vaginal environment is acidic and oxygen‑poor, which influences which antibiotics work best. Metronidazole and clindamycin are the front‑line drugs for bacterial vaginosis (BV). They target the anaerobic bacteria that dominate BV.
- Clindamycin - cream or oral tablets, 300 mg twice daily for 7 days.
- Metronidazole - 500 mg orally twice a day, or a 0.75% gel applied nightly for 5 days.
Both drugs can cause a temporary increase in yeast, so many clinicians prescribe an antifungal (like fluconazole) after the antibiotic course.
Balancing Efficacy and Safety - Pregnancy Considerations
Pregnant patients need extra caution. Some antibiotics are contraindicated because they can cross the placenta. Here’s a quick safety snapshot:
| Antibiotic | Pregnancy Category (US) | Typical Use | Key Warning |
|---|---|---|---|
| Metronidazole | B | Intestinal & vaginal anaerobes | Avoid first trimester if possible |
| Clindamycin | B | BV, skin infections | Monitor for C. diff risk |
| Amoxicillin | B | Urinary & respiratory bacteria | Generally safe, watch for allergy |
| Vancomycin (oral) | C | Severe C. diff | Use only when benefits outweigh risks |
When Antibiotics Aren’t the Answer
Not every gut or vaginal upset needs an antibiotic. Some diarrhea spells are viral, and many cases of BV improve with lifestyle changes (avoiding douches, using cotton underwear). Over‑prescribing antibiotics fuels resistance, which is a growing public‑health threat.
Key red flags that suggest a bacterial cause needing treatment include:
- Fever above 100.4 °F (38 °C) with abdominal pain.
- Frequent, watery stools that persist >3 days.
- Vaginal discharge that’s thin, gray‑white, and fishy‑smelling.
If you’re unsure, a stool culture or a vaginal swab can guide the doctor toward the right drug.
Managing Side Effects and Reducing Recurrence
Side effects are common because antibiotics disturb the normal flora. Here are practical steps to stay comfortable:
- Take the drug with food unless the label says otherwise.
- Stay hydrated - water helps flush toxins.
- Finish the full course, even if you feel better.
- Consider a probiotic supplement (e.g., Lactobacillus acidophilus) for 2 weeks after finishing the antibiotic.
To lower the chance of a repeat infection, keep good hygiene, practice safe food handling, and avoid unnecessary antibiotic courses.
Key Takeaways
- Antibiotics target specific bacteria; choose drugs that work in the low‑oxygen environment of the gut or vagina.
- Metronidazole and clindamycin are the most common choices for both intestinal and vaginal anaerobic infections.
- Pregnant patients need drugs with proven safety; metronidazole and clindamycin are generally acceptable after the first trimester.
- Side effects often include diarrhea or yeast overgrowth - probiotics and antifungals can help.
- Never use antibiotics for viral or non‑bacterial symptoms; testing can prevent unnecessary prescriptions.
Frequently Asked Questions
Can I use the same antibiotic for an intestinal infection and a vaginal infection?
Sometimes, yes. Metronidazole works well for both C. diff in the gut and bacterial vaginosis. However, dosage and treatment length differ, so only a doctor should decide.
What should I do if I develop a yeast infection after finishing antibiotics?
A short course of an over‑the‑counter antifungal (like fluconazole 150 mg) usually clears it. Adding a probiotic during and after antibiotics can also prevent yeast overgrowth.
Is it safe to take probiotics while on antibiotics?
Yes. Take the probiotic at least 2 hours after the antibiotic dose to give each product a chance to work.
How long does it take for C. diff symptoms to improve after treatment?
Most patients feel better within 3‑5 days, but the full course (usually 10 days) is needed to prevent recurrence.
Can over‑the‑counter antibiotics treat these infections?
In many countries antibiotics require a prescription because misuse contributes to resistance. Always see a healthcare professional before starting any course.
Next Steps for Different Readers
If you suspect an infection: schedule a doctor’s visit, request stool or vaginal testing, and discuss any allergies or pregnancy status.
If you’re already on antibiotics: follow the dosing schedule, stay hydrated, and start a probiotic within the first day of treatment.
If you’re a caregiver or health worker: educate patients about completing courses, avoiding self‑medication, and the importance of hygiene to curb spread.
Understanding how antibiotics work in each body region helps you make smarter choices and reduces the risk of resistance - a win for you and for public health.