When a doctor writes a prescription, they’re not just picking a medicine-they’re making a decision that affects your health, your wallet, and their own bottom line. And increasingly, that decision is being nudged-sometimes subtly, sometimes directly-by financial and non-financial rewards tied to prescribing generic drugs.
Why Do Providers Get Rewarded for Prescribing Generics?
The math is simple: generic drugs work just like brand-name drugs but cost a fraction of the price. In the U.S., generics make up 90% of all prescriptions but only 23% of total drug spending. That’s because they don’t carry the massive research and marketing costs that brand-name drugs do. Over the past 15 years, generics have saved the U.S. healthcare system more than $1.7 trillion. So it’s no surprise that insurers, Medicare, and large health systems are trying to get providers to write more of them. But here’s the catch: doctors aren’t paid based on how many prescriptions they write. They’re paid for seeing patients, managing chronic conditions, and delivering care. So if you want them to switch to generics, you have to give them a reason-beyond just doing the right thing. That’s where incentives come in.How Do These Incentives Actually Work?
There are two main types: financial and non-financial. Financial incentives are the most straightforward. Some health plans pay providers a bonus for each generic prescription they write. For example, Blue Cross Blue Shield plans have offered $5 to $15 per generic fill for certain drug classes, with top performers earning up to $5,000 a year. UnitedHealthcare’s Value-Based Prescribing Program pays primary care doctors based on how often they choose generics over brand names-resulting in a 24.7% increase in generic use in those practices. But it’s not all cash. Non-financial rewards matter too. Some systems give doctors priority scheduling for their patients if they consistently use generics. Others speed up prior authorization requests-something that used to take days and now takes minutes. A few even put providers on a ‘Wall of Fame’ in the clinic for high generic prescribing rates. These might sound small, but in a high-pressure environment, even a faster approval process can save hours of administrative work. Electronic systems play a big role too. Most EHRs now default to showing generic alternatives first when a doctor starts typing a prescription. One study found this simple change increased generic prescribing by over 22 percentage points. It doesn’t force the doctor’s hand-it just makes the cheaper, equally effective option easier to pick.What’s the Evidence That It Works?
The numbers don’t lie. When incentives are well-designed, usage goes up. Medicare’s ‘$2 Drug List’-which capped copays for essential generics at $2-led to a 17.3% jump in adherence among seniors. In Germany, where the system sets reimbursement based on the cheapest effective drug in a class, 93% of off-patent prescriptions are generics. In the U.S., that number is 85%. And in practices that combined e-prescribing defaults with education, generic use jumped by 18.5 percentage points. But not every program works the same. Formulary tiering-where generics are placed in the lowest-cost tier-is common, but it mostly shifts cost to patients, not providers. It only increases generic use by 8-12%. Direct provider incentives? Those move the needle much more.
Where Things Get Complicated
It’s not all smooth sailing. Some providers feel pressured. Dr. Sarah Williams, a family doctor in Texas, told Medscape in 2022 that some incentive programs feel like they’re forcing her to choose cost over clinical judgment. And she’s not alone. On Reddit, a physician named MedDoc2020 wrote: “Generic incentives work fine for simple cases. But when a patient has five chronic conditions and needs a specific brand because of how they metabolize drugs? That’s when it gets dangerous.” There’s also a darker side. Studies show that doctors who receive payments from pharmaceutical companies-even small ones like free meals or educational materials-are 37% less likely to prescribe generics, especially for newer ones. And in some cases, the system backfires. Clinics that qualify for the 340B drug discount program (which gives them deep discounts on brand-name drugs) actually prescribed generics less often than others. Why? Because they were getting such good deals on the expensive stuff, the financial incentive to switch vanished. Even more concerning: when patients find out their doctor is being paid to prescribe generics, trust can erode. A 2021 MGMA survey found that 78% of providers worried about patient reactions if incentives were disclosed. That’s a real risk. If a patient thinks their doctor is choosing a drug because of a bonus, not because it’s right for them, the relationship suffers.What Makes a Good Incentive Program?
The best programs don’t just push for cost savings-they protect clinical freedom. The American College of Physicians (ACP) recommends three key rules:- Only reward prescribing when generics are clinically appropriate-not for every drug, every time.
- Exclude medications where brand formulation matters-like epilepsy drugs or thyroid meds-where small differences in absorption can cause harm.
- Frame incentives as quality metrics, not cost-cutting mandates.
Who’s Winning and Who’s Losing?
Primary care doctors are the biggest winners. They handle the most routine prescriptions-high blood pressure, diabetes, cholesterol-and generics make up nearly 90% of their scripts. Specialists? Not so much. Cardiologists, neurologists, and oncologists prescribe generics at lower rates (76% vs. 89% for primary care), because their patients often need specific formulations or newer drugs that don’t yet have generic versions. Pharmacy benefit managers (PBMs)-like CVS Caremark and OptumRx-control 78% of the prescription drug market. They design the formularies, set the tiers, and decide which incentives get paid out. So while the goal is cost savings, the real power lies with these middlemen, not the doctors or patients.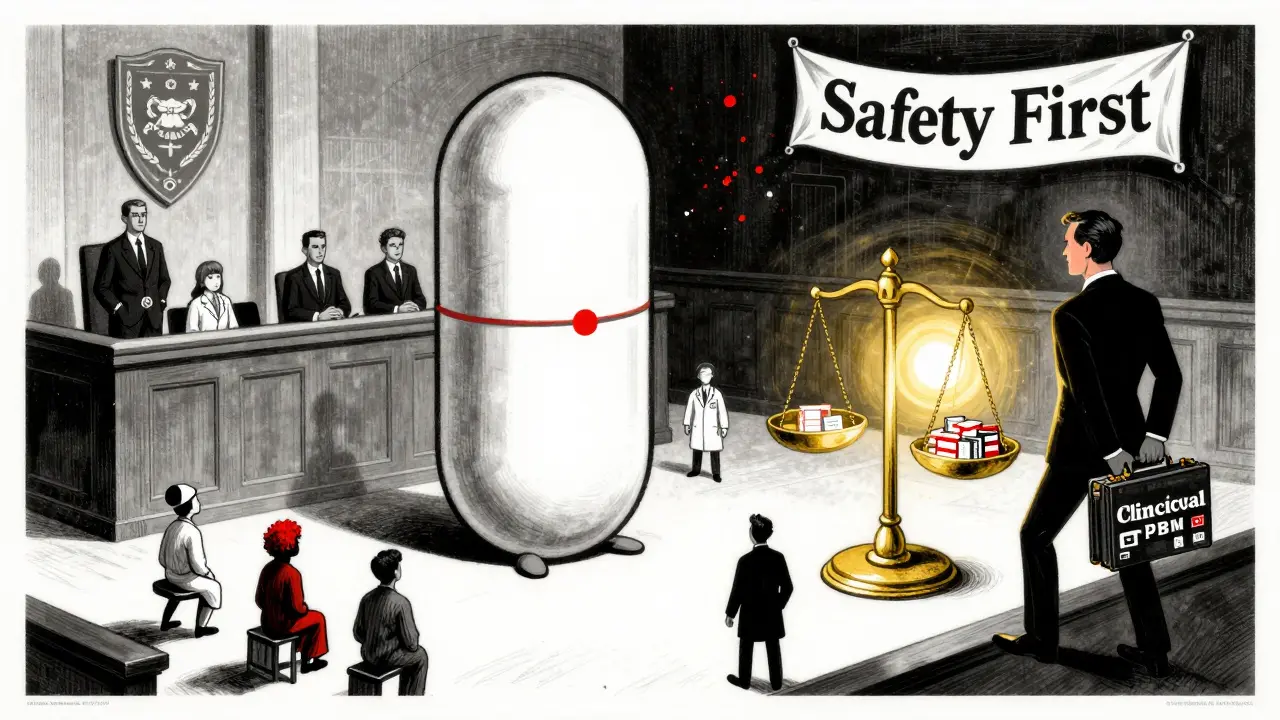
What’s Next?
The future is moving toward outcomes-based incentives. UnitedHealthcare’s 2024 rollout of value-based prescribing contracts will tie payments not just to how many generics are prescribed, but to whether patients stay on their meds, avoid hospital visits, and improve their health. That’s a smarter approach. It rewards good outcomes, not just cheap prescriptions. The Inflation Reduction Act of 2022 is also pushing patent reform to make it easier for generics to enter the market. Experts predict this could bump U.S. generic use from 90% to 94% by 2028. But the biggest challenge isn’t technology or policy-it’s trust. If providers feel like they’re being manipulated, or if patients feel like they’re being treated like a line item on a balance sheet, the whole system loses. The goal shouldn’t be to maximize generic prescriptions. It should be to maximize good care-affordable, safe, and personalized.What Should You Do as a Patient?
You don’t need to understand the inner workings of insurance formularies. But you do need to ask questions. If your doctor suggests a generic, ask: “Is this safe for me? Are there any reasons I should stick with the brand?” If they’re hesitant, or if you’re on a complex regimen, speak up. You have the right to know why a drug is being chosen. And if you’re on a fixed income, ask if your plan has a $2 or $5 generic list. Many do. You could save hundreds a year.Final Thoughts
Generic prescribing incentives aren’t perfect. They can be misused. They can create conflicts. But they’re also one of the most effective tools we have to bring down the cost of medicine without sacrificing quality. The key is designing them right-transparently, ethically, and with clinical judgment at the center. The system isn’t broken. It just needs better guardrails. And the people who know best how to use them? The doctors. The patients. And the people who care enough to ask the right questions.Do generic drugs work as well as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They’re tested to prove they work the same way in the body. The only differences are in inactive ingredients like fillers or dyes-which rarely affect how the drug works. The FDA requires generics to be bioequivalent, meaning they deliver the same amount of medicine into your bloodstream at the same rate.
Why do some doctors resist prescribing generics?
Some doctors worry that one-size-fits-all incentives ignore patient complexity. For example, patients with epilepsy, thyroid disorders, or mental health conditions may need a specific brand because of how their body absorbs the drug. Others feel pressured by financial targets that don’t account for clinical nuance. A 2023 study found that 52% of implementation failures were due to provider resistance tied to perceived threats to autonomy.
Are generic prescribing incentives ethical?
It depends on how they’re designed. Incentives that reward cost savings without considering clinical appropriateness can be unethical. But when they’re tied to quality, transparency, and patient outcomes-like improved adherence or fewer hospital visits-they’re aligned with good medical practice. The key is avoiding hidden payments from drug companies and making sure incentives don’t override clinical judgment.
Can patients benefit financially from generic prescribing?
Absolutely. Generic drugs often cost 80-85% less than brand names. For patients on Medicare Part D, many plans offer a $2 or $5 copay list for essential generics. A patient taking a $300/month brand-name drug could switch to a $15 generic and save $3,420 a year. Even with insurance, lower copays mean fewer people skip doses or stop taking their meds altogether.
Do all insurance plans offer provider incentives for generics?
Most do. As of 2023, 89% of U.S. health plans include some form of provider incentive for generic prescribing. These range from simple formulary tiering to direct bonuses and performance-based contracts. Large insurers like UnitedHealthcare, Blue Cross, and Anthem lead the way, but even smaller regional plans are adopting them. Medicare Advantage plans are also rolling out similar programs under CMS’s Innovation Center initiatives.
What’s the difference between formulary tiering and direct provider incentives?
Formulary tiering shifts cost to the patient. It makes generics cheaper for you, but doesn’t pay the doctor anything. Direct provider incentives pay the doctor for choosing generics-so they’re motivated to pick them. Tiering increases generic use by 8-12%. Direct incentives? They’ve been shown to increase use by over 24%. The latter works better because it changes provider behavior, not just patient cost-sharing.
Do generic incentives lead to worse care?
Not if they’re designed well. Poorly designed programs that force generic use in cases where brand drugs are medically necessary can lead to errors. But the best programs use clinical decision support to flag when a brand is needed-and exclude those drugs from incentives. A 2023 JAMA study found that when incentives were paired with appropriate exclusions and education, there was no increase in adverse events.
How do I know if my doctor is being paid to prescribe generics?
You usually won’t know. Most programs don’t disclose this to patients, and many providers don’t even think about it-it’s just part of how the system works. But if you’re concerned, ask: “Is this the best option for me, or is there a financial reason you’re recommending it?” A good doctor will welcome the question and explain their reasoning without defensiveness.
