Neuroblastoma Treatment Options Calculator
Treatment Selection Tool
Identify potential treatment options based on your child's specific genetic markers and disease characteristics.
Recommended Treatment Options
Every parent of a child diagnosed with neuroblastoma knows that the fight feels endless. Yet the landscape is shifting fast-new genetics, smarter drugs, and immune‑based tricks are turning a once‑hopeless disease into a battlefield where scientists are gaining real ground. This article walks you through the biggest advances on the horizon, why they matter, and what families can realistically expect in the next few years.
Key Takeaways
- Genomic profiling now identifies actionable targets in up to 60% of high‑risk cases.
- CAR‑T cells and GD2‑directed antibodies are moving from trials to early approvals, offering targeted neuroblastoma treatment options.
- Liquid biopsy and AI‑driven imaging enable real‑time monitoring of disease response.
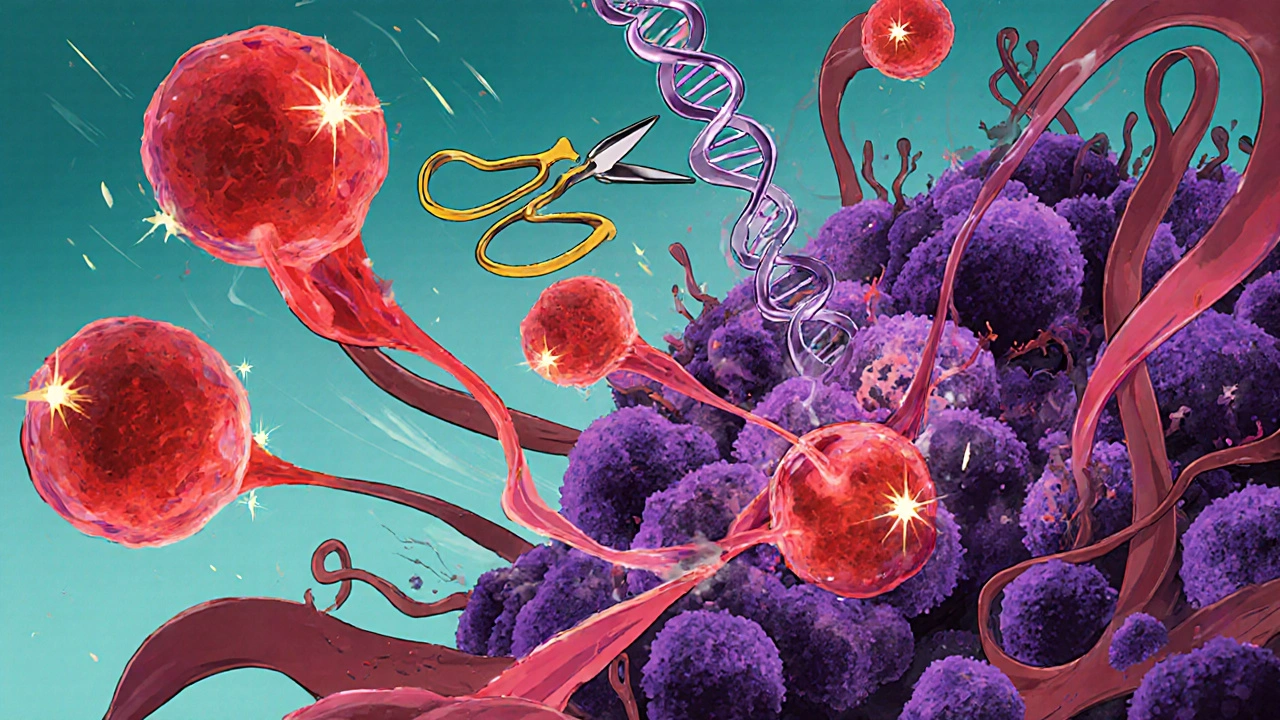
- CRISPR‑based gene editing shows promise for correcting driver mutations like ALK.
- Access and cost remain major hurdles; advocacy and clinical‑trial enrollment are crucial.
Understanding Neuroblastoma
Neuroblastoma is a rare pediatric cancer that originates from immature nerve cells (neuroblasts) in the sympathetic nervous system. It accounts for about 7% of childhood cancers but causes roughly 15% of cancer‑related deaths in kids under five. The disease is notorious for its heterogeneity: some tumors shrink spontaneously, while others become aggressive and spread to bone marrow, liver, and brain. Early detection and precise staging are vital, but many cases present at an advanced stage, limiting cure rates.
Recent Milestones in the Science
Over the past decade, three scientific breakthroughs reshaped how researchers view neuroblastoma.
- Genomic profiling. Whole‑exome sequencing revealed that MYCN amplification, present in ~20% of cases, drives rapid growth. Simultaneously, activating ALK mutations (found in 8-10% of patients) opened a drug‑targetable window.
- Immunotherapy breakthroughs. The first FDA‑approved GD2‑targeted antibody (dinutuximab) improved 3‑year event‑free survival from 40% to 57% in high‑risk patients.
- Precision medicine platforms. Multi‑omic panels now combine DNA, RNA, and epigenetic data, allowing clinicians to match patients with tailored clinical trials.
Emerging Therapeutic Frontiers
While the above advances set the stage, several novel approaches are racing toward clinical use.
- CAR‑T cell therapy. Engineers modify a patient’s T‑cells to recognize GD2 on neuroblastoma cells. Early‑phase studies report response rates above 70% in refractory disease, with manageable cytokine release syndromes.
- Next‑generation GD2 antibodies. Bispecific antibodies link GD2 to immune cells, amplifying cytotoxicity while reducing neuropathic pain.
- ALK inhibitors. Drugs like lorlatinib and ensartinib, originally approved for lung cancer, are being repurposed for ALK‑mutant neuroblastoma, showing partial responses in 30-40% of patients.
- Epigenetic modulators. BET‑ bromodomain inhibitors and EZH2 blockers re‑activate tumor suppressor genes, sensitizing tumors to chemotherapy.
- Liquid biopsy technologies now detect circulating tumor DNA (ctDNA) and RNA, enabling non‑invasive monitoring of mutation burden and treatment response.
Comparing the Most Promising Emerging Therapies
| Therapy | Mechanism | Clinical Stage (2025) | Target Population | Typical Side Effects |
|---|---|---|---|---|
| CAR‑T (GD2‑directed) | Engineered T‑cells recognize GD2 surface antigen | Phase II/III | Refractory/high‑risk, GD2‑positive | Cytokine release, neurotoxicity (mild) |
| Bispecific GD2 antibody | Links GD2 to CD3 on T‑cells | Phase II | Newly diagnosed high‑risk | Pain, infusion reactions |
| ALK inhibitor (lorlatinib) | Blocks ALK tyrosine‑kinase activity | Phase III | ALK‑mutated tumors | Liver enzyme elevation, hyperlipidemia |
| BET‑bromodomain inhibitor | Disrupts transcription of oncogenes | Phase I/II | MYCN‑amplified, resistant disease | Thrombocytopenia, fatigue |
| Liquid biopsy‑guided therapy | Real‑time ctDNA monitoring to adjust regimen | Clinical validation ongoing | All stages, especially relapsed | Minimal (blood draw) |
Precision Medicine and Real‑Time Monitoring
The integration of liquid biopsy into standard care is a game changer. Instead of waiting weeks for a tissue biopsy, doctors can track ctDNA levels weekly, catching minimal residual disease before imaging shows a relapse. AI algorithms analyze mutation trends and suggest treatment switches-often moving patients from standard chemotherapy to a targeted ALK inhibitor within days.

Gene Editing: CRISPR’s Role on the Horizon
CRISPR‑Cas9 technology is no longer confined to the lab bench. Early animal models demonstrate that excising the MYCN amplification segment halts tumor growth without harming normal tissue. Human trials are expected by 2027, focusing on ex vivo editing of patient‑derived hematopoietic stem cells to deliver anti‑tumor immunity. While safety and off‑target effects remain concerns, the potential to correct driver mutations at their source is stirring excitement across oncology conferences.
Challenges, Ethics, and Access
Science moves fast, but equity moves slower. Cutting‑edge therapies often cost six to eight figures per patient, and many families lack insurance coverage for experimental protocols. Moreover, the tumor microenvironment-the surrounding immune cells and stromal fibers-still thwarts many immunotherapies, demanding combination approaches that add complexity and expense.
Ethical debates swirl around gene editing in children. While correcting a fatal mutation sounds noble, regulators caution against germline changes that could affect future generations. For now, most CRISPR efforts remain somatic-targeted only to the patient’s tumor cells.
What Families Can Expect in the Next 5Years
- Broader trial access. Cooperative groups are creating umbrella protocols that allow patients to be screened centrally for any targetable alteration, reducing travel and wait times.
- Combination regimens. Expect FDA approvals for CAR‑T plus GD2 antibody combos, aiming to attack the tumor from multiple angles.
- Home‑based monitoring. Portable ctDNA kits could let parents send a blood spot to a lab weekly, receiving automated alerts if disease markers rise.
- Insurance evolution. As outcomes improve, payers are beginning to reimburse personalized therapies under value‑based contracts.
- Increased survivorship support. Long‑term follow‑up clinics are expanding, focusing on neurocognitive health, endocrine function, and secondary cancer screening.
In short, the future blends cutting‑edge biology with smarter delivery. While challenges remain, the odds of turning a high‑risk neuroblastoma diagnosis into a chronic, manageable condition are better than ever.
Frequently Asked Questions
What is the current survival rate for high‑risk neuroblastoma?
Five‑year event‑free survival for high‑risk patients is roughly 50% with standard therapy, but trials adding immunotherapy push that number toward 65%.
How does CAR‑T therapy differ from traditional chemotherapy?
CAR‑T uses a patient’s own T‑cells engineered to hunt tumor‑specific proteins, offering a targeted attack with fewer systemic side effects than chemo, which wipes out both cancer and healthy rapidly dividing cells.
Can a liquid biopsy replace tissue biopsy?
Not completely. Liquid biopsy excels at monitoring disease dynamics and detecting mutations, but a tissue sample is still needed for initial histology and full molecular profiling.
Are ALK inhibitors safe for children?
Early pediatric trials report manageable toxicity, mainly liver enzyme elevation and lipid changes. Ongoing studies are refining dosing to balance efficacy and safety.
What role does CRISPR play in future treatments?
CRISPR aims to edit or knock out driver genes like MYCN directly in tumor cells. Human trials are still years away, but animal data suggest it could halt tumor growth without harming normal tissue.
