Celiac Disease Risk Assessment Tool
Assess Your Risk
This tool helps you understand your potential risk of celiac disease based on symptoms and family history. Not a diagnosis - always consult your doctor for medical advice.
Ever felt a burning or tight knot right under your breastbone and wondered why? That discomfort is called Epigastric Pain is pain located in the upper central region of the abdomen, just below the sternum. While many blame heartburn or stress, a less obvious culprit is celiac disease. Understanding how an autoimmune reaction to gluten can trigger that nagging ache helps you avoid misdiagnosis and get relief faster.
What Is Epigastric Pain?
Epigastric pain sits in the "upper belly" - the area called the epigastrium. It can feel like a dull ache, sharp stab, burning sensation, or even a pressure that mimics heart issues. Common triggers include acid reflux, gastritis, and ulcers. However, the pain’s location doesn’t tell you the root cause; you need to look at accompanying signs and your medical history.
How Celiac Disease Triggers Epigastric Pain
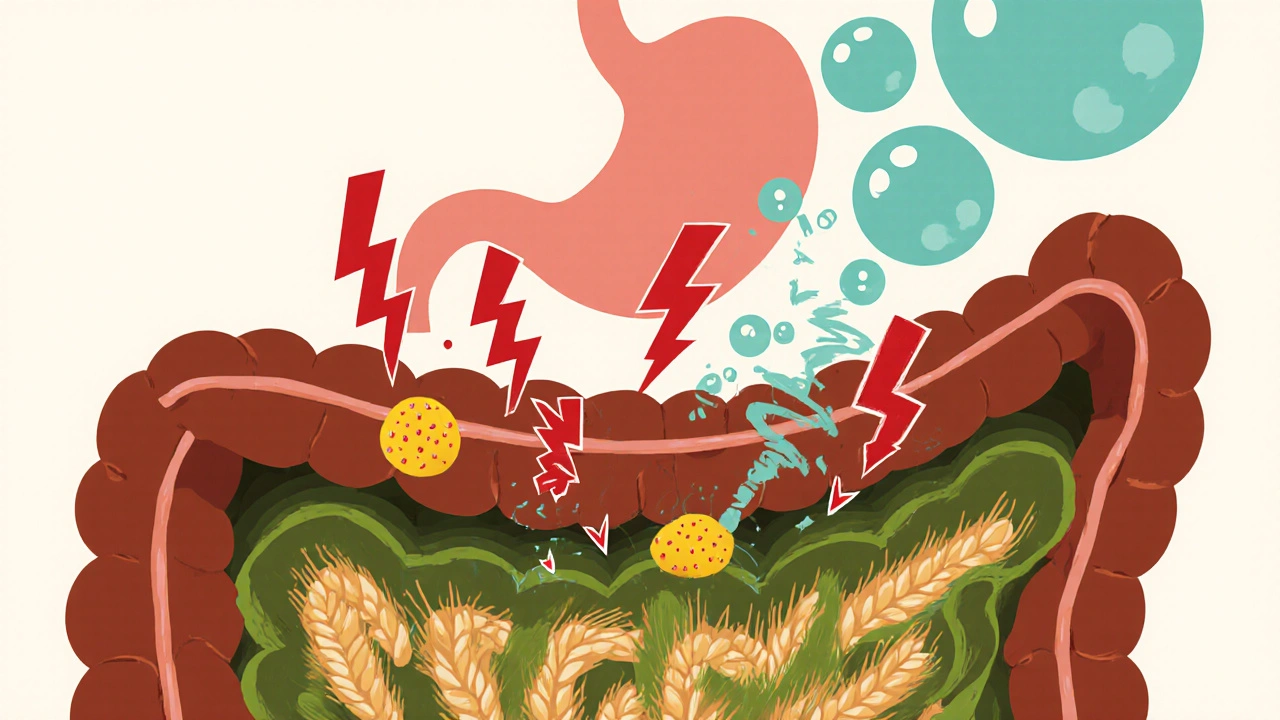
Celiac Disease is an autoimmune disorder where ingestion of gluten leads to damage of the small intestine’s lining. When you eat wheat, barley, or rye, the immune system launches an attack on the mucosal surface, causing inflammation that can radiate upward and be felt as epigastric pain.
- Autoimmune reaction: The body produces antibodies (anti‑tTG, anti‑EMA) that damage the villi, the tiny finger‑like projections that absorb nutrients.
- Malabsorption: With villous atrophy, nutrients like iron and B12 aren’t absorbed, leading to anemia, fatigue, and sometimes pain due to muscle cramping.
- Gas and bloating: Undigested gluten ferments in the colon, creating excess gas that pushes against the stomach, intensifying epigastric discomfort.
Because the pain feels generic, many patients are first treated for gastritis or reflux, delaying the correct diagnosis.
Beyond Pain: Typical Symptoms of Celiac Disease
If you’ve ever wondered why you’re constantly tired, have unexplained weight loss, or keep getting skin rashes, consider the broader symptom list:
- Chronic diarrhea or constipation
- Flat, itchy skin rash called dermatitis herpetiformis
- Iron‑deficiency anemia that doesn’t improve with supplements
- Joint pain or osteoporosis
- Neurological issues such as peripheral neuropathy
Not everyone experiences the classic "classic" signs. Some people, especially adults, present only with vague abdominal discomfort like epigastric pain.
How Doctors Diagnose Celiac Disease When Epigastric Pain Is the Main Complaint
When a patient reports epigastric pain, physicians follow a step‑by‑step protocol to rule out other causes and then check for celiac disease if red flags appear.
| Step | What Happens | Why It Matters |
|---|---|---|
| 1. Clinical Evaluation | Review diet, family history, and extra‑intestinal symptoms | Helps identify risk factors like HLA‑DQ2/DQ8 genes |
| 2. Serology Tests | Blood tests for anti‑tTG IgA, EMA, and total IgA | Positive results strongly suggest celiac disease |
| 3. Genetic Testing | Check for HLA‑DQ2 or HLA‑DQ8 alleles | Absence virtually rules out celiac disease |
| 4. Endoscopic Biopsy | Take 4‑6 samples from the duodenum | Look for villous atrophy, crypt hyperplasia, and intraepithelial lymphocytes |
| 5. Gluten Challenge (if needed) | Re‑introduce gluten under medical supervision | Confirms symptom recurrence and guides treatment |
Doctors also order tests to exclude other epigastric pain sources: H. pylori breath test, upper GI endoscopy for ulcers, and abdominal ultrasound for gallbladder disease.
Managing Epigastric Pain With a Gluten‑Free Lifestyle
Once celiac disease is confirmed, the single most effective treatment is a strict gluten‑free diet (GFD). Here’s how it helps:
- Reduces inflammation: No more immune attacks on the small intestine means the villi can start healing.
- Improves nutrient absorption: Iron, calcium, and vitamin D levels rise, decreasing fatigue and muscle cramps that can aggravate pain.
- Less gas production: Without gluten fermentation, bloating subsides, easing pressure on the epigastric region.
Practical tips for staying gluten‑free:
- Read labels for hidden gluten (e.g., malt, modified food starch, hydrolyzed vegetable protein).
- Choose naturally gluten‑free grains: rice, quinoa, buckwheat, and certified gluten‑free oats.
- Beware of cross‑contamination in kitchens, especially when sharing cooking space with wheat‑eaters.
- Use a mobile app to scan barcodes and verify ingredients on the go.
- Schedule follow‑up serology tests after 6‑12 months to confirm antibody levels are dropping.
Most patients report a noticeable drop in epigastric pain within weeks of eliminating gluten, though complete intestinal healing can take up to two years.

When to Seek Immediate Medical Attention
While a GFD often eases discomfort, certain warning signs demand urgent care:
- Sudden, severe chest pain that radiates to the arm or jaw (rule out cardiac events).
- Persistent vomiting, especially if accompanied by dehydration.
- Unexplained weight loss >10 % of body weight over a short period.
- New onset neurological symptoms like numbness or severe headaches.
If any of these appear, call emergency services or visit the nearest urgent care center.
Common Misconceptions About Epigastric Pain and Celiac Disease
Myths can keep people from getting proper help.
- Myth: Only kids get celiac disease.
Fact: Adults make up the majority of new diagnoses, often presenting with vague abdominal pain. - Myth: If you feel better after a few weeks of a GFD, you’re cured.
Fact: Lifelong adherence is required; occasional gluten exposure can reignite damage. - Myth: Gluten‑free processed foods are automatically healthy.
Fact: Many GF snacks are high in sugar and saturated fats; focus on whole foods.
Clearing these misconceptions empowers you to talk confidently with your doctor and stick to an effective treatment plan.
Quick Checklist for Anyone With Epigastric Pain Suspecting Celiac Disease
- Track food intake and symptom timing for at least two weeks.
- Note any extra‑intestinal signs: anemia, skin rash, joint pain.
- Ask your clinician for serology tests (tTG IgA, total IgA).
- If blood work is positive, schedule an endoscopy with biopsy.
- Start a gluten‑free trial only after testing; don’t self‑diagnose.
Can epigastric pain be the only symptom of celiac disease?
Yes. Some adults experience only upper‑abdominal discomfort without classic diarrhea or weight loss. That’s why doctors consider celiac testing when pain persists despite standard reflux treatment.
How long does it take for epigastric pain to improve after starting a gluten‑free diet?
Most people notice relief within 2‑4 weeks, but full intestinal healing can require 12‑24 months, especially if damage was severe.
Do I need to avoid oats completely?
Pure, certified gluten‑free oats are generally safe for most celiac patients, but a small subset reacts to avenin. Test tolerance under medical guidance.
What other conditions can mimic epigastric pain caused by celiac disease?
Common mimics include gastroesophageal reflux disease (GERD), peptic ulcer disease, functional dyspepsia, gallbladder disease, and early pancreatitis.
Is a gluten‑free diet enough if I also have lactose intolerance?
Lactose intolerance often co‑exists with celiac disease because damaged villi reduce lactase production. You may need to limit dairy or use lactase supplements alongside the gluten‑free diet.
