Drug Withdrawal Status Checker
Check if Your Medication is Withdrawn
Enter a drug name to see if it's been withdrawn by the FDA and why.
Enter a drug name above to check its withdrawal status.
Important: This tool checks a limited database of known withdrawn drugs. Always verify with the FDA's official "Determination of Safety or Effectiveness" list for the most current information.
For comprehensive information, visit the FDA's official drug withdrawal list: FDA Drug Safety Communications
Why Do Drugs Get Pulled from the Market?
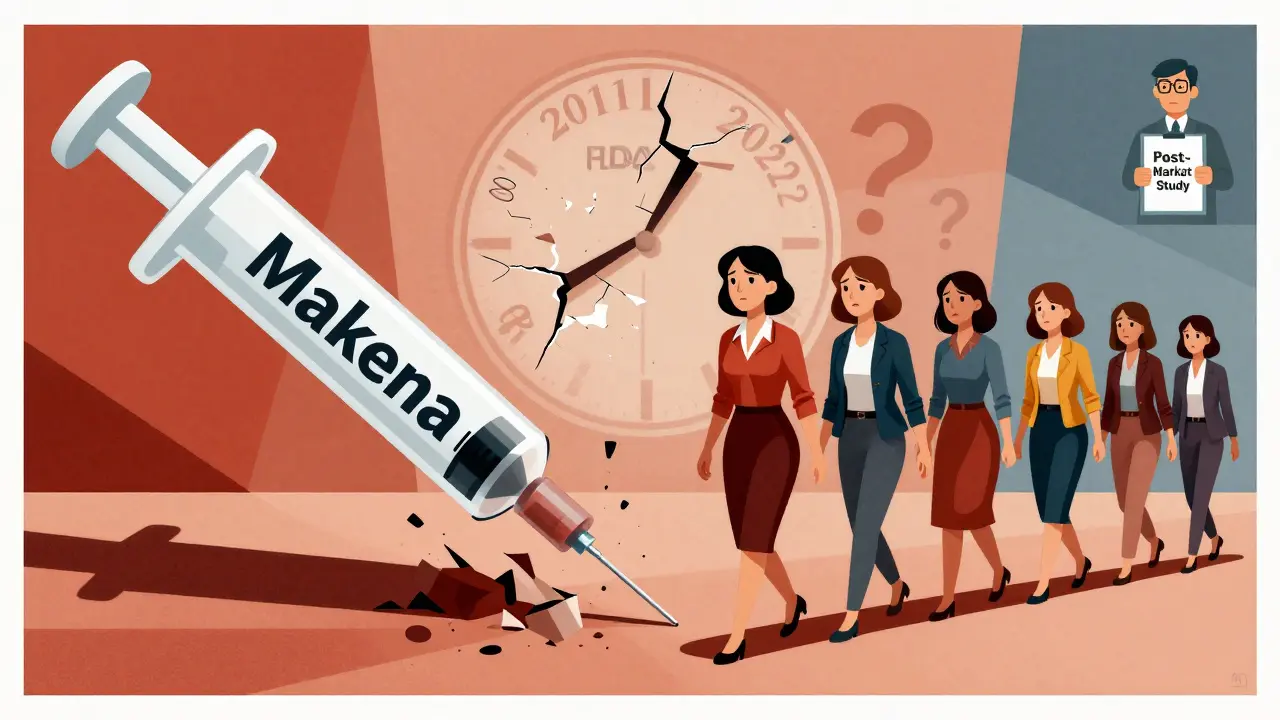
It’s easy to assume that if a drug is approved by the FDA, it’s safe and works as promised. But that’s not always true. Every year, some medications are pulled from shelves-not because they’re defective, but because new evidence shows they don’t work as claimed, or worse, they cause unexpected harm. The most infamous case is Makena, a drug approved in 2011 to prevent preterm birth in high-risk women. Four years later, a follow-up study proved it didn’t work. Yet the drug stayed on the market for another 11 years, until 2022. During that time, an estimated 150,000 women received a treatment that offered no benefit, only cost and risk.
The Difference Between Voluntary and Mandatory Withdrawals
Not all drug removals are the same. There are two main types: voluntary and mandatory. Voluntary withdrawals happen when a drugmaker decides on its own to stop selling a product. This could be due to low sales, manufacturing issues, or emerging safety signals. But if the FDA finds clear evidence of danger or ineffectiveness, it can force a mandatory withdrawal. That’s where things get serious.
The FDA doesn’t act on rumors or isolated reports. It requires solid data-usually from post-market studies, real-world patient outcomes, or independent research. In 2023, Congress gave the FDA new power to speed up these decisions. Before, the agency could take years to act. Now, under the Consolidated Appropriations Act of 2023, the process has clear steps: the FDA must notify the company, give them a chance to respond, hold a meeting, and make a final decision within 180 days. That’s a big shift from the old system, where some drugs lingered on shelves for over four years after being proven useless.
Accelerated Approval: Faster Access, Bigger Risks
Many drugs pulled from the market were approved under the FDA’s accelerated pathway. This program was designed to get life-saving treatments to patients with serious illnesses-like cancer or rare diseases-faster. Instead of waiting for long-term survival data, the FDA lets companies use early signs of benefit, like tumor shrinkage, to get approval. The catch? They must later prove the drug actually improves how long patients live or how well they feel.
But here’s the problem: too many companies never do that follow-up work. A 2023 study from the Penn LDI found that 26% of drugs approved under accelerated pathways were eventually withdrawn for lack of effectiveness. In small cell lung cancer, 41% of patients received drugs later pulled from the market. That’s not just a statistic-it’s a person sitting in a clinic, getting a treatment that was never proven to help.

What Triggers a Withdrawal?
The FDA won’t pull a drug unless one of four things happens:
- The company fails to complete required post-approval studies on time.
- The follow-up study shows the drug doesn’t deliver the promised benefit.
- Independent research or patient data proves the drug is unsafe or ineffective.
- The company lied or misled doctors and patients about the drug’s benefits.
These rules were formalized in 2023, but they’ve been ignored for too long. Take Makena again. The FDA approved it based on a small study showing it reduced preterm birth by a few percentage points. But no study ever showed it saved babies’ lives or improved long-term outcomes. The company didn’t run the required study for over a decade. By the time the FDA acted, the damage was done.
How Patients and Doctors Get Affected
When a drug is pulled, it doesn’t vanish overnight. Pharmacies still have stock. Doctors keep prescribing it because they don’t get clear warnings. A 2023 FDA audit found that only 42% of withdrawal notices included guidance on how to switch patients to safer alternatives. That leaves doctors guessing.
Patient communities are filled with stories of confusion and betrayal. One woman with metastatic breast cancer posted on a support forum: “I was on [withdrawn drug] for 18 months. My oncologist said it was standard care. Now I’m told it did nothing.” She wasn’t alone. A survey by the Patient Advocate Foundation found 78% of patients believe the FDA takes too long to remove ineffective drugs.
Healthcare providers are frustrated too. Oncology clinics report it takes an average of 72 hours to find a replacement therapy after a drug is withdrawn. In cancer care, those 72 hours can mean the difference between hope and decline.
The Orange Book and What It Really Means
Doctors and pharmacists rely on the FDA’s Orange Book-a public list of approved drugs and their patent status. But here’s the catch: the Orange Book doesn’t automatically update when a drug is withdrawn. The FDA publishes a separate “Determination of Safety or Effectiveness” list in the Federal Register, but most prescribers don’t check it. A 2022 survey found 63% of pharmacists struggled to interpret which drugs were truly withdrawn versus just temporarily out of stock.
That’s dangerous. A drug that’s been pulled for safety reasons can’t be used as a reference for generic versions. But if a pharmacist doesn’t know the difference, they might dispense a generic version of a drug that should never have been approved in the first place.

How the System Is Changing-And Why It Matters
The 2023 law didn’t just tweak a rule-it changed the entire culture around drug safety. For the first time, the FDA has a real timeline. It created a dedicated team of 12 scientists and doctors just to handle accelerated approval withdrawals. Their goal? Cut the average withdrawal time from 46 months to under 12.
The first drug pulled under the new rules was an ALS treatment in August 2023. It didn’t work. The FDA acted fast. That’s progress.
But the real test is ahead. The FDA is now testing real-world data from Flatiron Health, which tracks millions of patient records, to spot ineffective drugs before formal studies even finish. If this works, we might stop waiting for clinical trials to catch up with reality.
What’s Next? The Balance Between Speed and Safety
Some drugmakers warn that faster withdrawals could scare off innovation. If companies fear their drugs will be pulled the moment a study goes sideways, they might stop trying to treat rare or aggressive diseases. That’s a real concern. But the bigger risk is doing nothing.
Right now, the system rewards speed over proof. The 2023 reforms don’t stop innovation-they demand accountability. If a drug is approved fast, it must be proven fast. No more waiting a decade to find out it didn’t work.
The goal isn’t to remove every drug that has a risk. It’s to remove the ones that offer no benefit at all. Because patients deserve more than hope. They deserve evidence.
Can a drug be pulled even if it’s been on the market for years?
Yes. The FDA can withdraw a drug at any time if new evidence shows it’s unsafe or ineffective. Makena was approved in 2011 and pulled in 2022 after a long-delayed study proved it didn’t work. The length of time on the market doesn’t protect a drug from being removed.
What’s the difference between a recall and a withdrawal?
A recall is when a specific batch or lot of a drug is removed due to contamination, mislabeling, or manufacturing defects. A withdrawal is when the entire drug is pulled from the market because it’s unsafe or ineffective for its intended use. Withdrawals are about the drug itself-recalls are about the product.
How do I know if a drug I’m taking has been withdrawn?
Check the FDA’s website for the “Determination of Safety or Effectiveness” list, which is updated monthly. You can also ask your pharmacist or doctor. But don’t rely on your pharmacy’s system alone-many don’t update in real time. If your drug is on the FDA’s withdrawal list, ask for alternatives immediately.
Are generic versions of withdrawn drugs still available?
No. Once a brand-name drug is withdrawn for safety or effectiveness reasons, generic versions cannot be approved or sold as substitutes. The FDA removes the drug from the list of approved reference products. If you’re prescribed a generic version of a withdrawn drug, it’s likely an error.
Why do some drugs stay on the market so long after being proven ineffective?
Before 2023, the FDA had no legal deadline to act. Companies often delayed submitting required studies, and the agency lacked the authority to force a quick decision. In some cases, political pressure, patient advocacy, or fear of backlash slowed the process. The new law closes those gaps by setting clear timelines and consequences for noncompliance.
Can I get compensation if I was harmed by a withdrawn drug?
Compensation is possible, but it’s complicated. You’d need to prove direct harm caused by the drug and that the manufacturer or FDA failed in their duty. Most cases are handled through civil lawsuits, not government programs. Patient advocacy groups like the Cancer Research Institute offer resources to help navigate these claims.
What You Can Do
If you’re on a medication for a serious condition-especially cancer, ALS, or rare diseases-ask your doctor: “Has this been tested in a confirmatory trial? Is it still on the FDA’s approved list?” Don’t assume it’s safe just because it’s prescribed. Keep records of your prescriptions and check the FDA’s withdrawal list every six months. If you find your drug has been pulled, contact your provider right away. You’re not just a patient-you’re your own best advocate.