Every year, over 1.3 million people in the U.S. end up in the emergency room because they took their medicine wrong. Not because they were careless. Not because they didn’t care. But because the label on their pill bottle didn’t make sense.
You’ve been there. You pick up your prescription, glance at the tiny print, and think, "Take one by mouth twice daily." But what does that really mean? Twice a day-morning and night? Or every 12 hours? What if it says "take with food"? Does that mean right after a meal? Or just anytime you eat something? And what about "q6h"? Is that four times a day? Or six? You’re not alone. Nearly half of all adults misunderstand at least one instruction on their prescription label.
What’s Actually on the Label (And Why It’s Confusing)
Most prescription labels were designed for pharmacists, not patients. They use abbreviations like "BID," "QHS," or "PO"-terms that mean nothing to someone without medical training. Even simple phrases like "take as needed" can be dangerous. One patient took her painkiller every two hours because she thought "as needed" meant "whenever I feel even a little ache." She ended up with liver damage.
Studies show that 27% of prescription instructions are written at a reading level higher than high school. That’s a problem when 36% of U.S. adults have basic or below-basic health literacy. Labels often skip key details: no mention of whether to take it before or after eating, no clear time frames, no explanation of what "daily" actually means in real life.
And the icons? The little pictures meant to help? Many are misleading. One common symbol-a plate with a fork-was meant to say "take with food." But 68% of patients thought it meant "take instead of food." That’s not helpful. That’s risky.
The Most Common Mistakes (And How They Happen)
Here are the top five misunderstandings you’re likely to run into:
- "Take once daily" vs. "Take once" - Some patients think "take once" means one pill total, not one pill every day. They take it on day one and forget the rest.
- "Twice daily" means every 12 hours - But many people think it means morning and bedtime, which is fine… unless they’re on antibiotics that need steady levels in the blood. Taking it at 8 a.m. and 8 p.m. is okay. Taking it at 8 a.m. and 6 p.m. isn’t always enough.
- "Take every 4 to 6 hours" - This sounds flexible, but patients often interpret it as "whenever I feel pain." That leads to overuse. One man took his ibuprofen every 3 hours for three days because he thought "every 4 to 6" meant "as often as possible." He got stomach bleeding.
- "Take with food" - Some think it means eat food right after taking the pill. Others think it means take it only if you’re eating. The truth? It means take it while eating or right after. This matters for drugs that irritate the stomach.
- Abbreviations like "q6h" - "q6h" means every six hours, which equals four times a day. But patients see "6" and think "six times." One Reddit user took his antibiotic four times a day thinking "q6h" meant "four times" because 24 divided by 6 is 4. He didn’t realize it meant every six hours. He ended up in the ER.
These aren’t just small mistakes. They lead to hospitalizations, organ damage, and even death.
How Pharmacies Are Trying to Fix This
Not all pharmacies are the same. Big chains like CVS, Walgreens, and Walmart have started using clearer labels. Their new designs include:
- Full words instead of abbreviations: "Take 1 tablet by mouth two times each day" instead of "1 tab BID."
- Specific times: "Take one in the morning and one at bedtime."
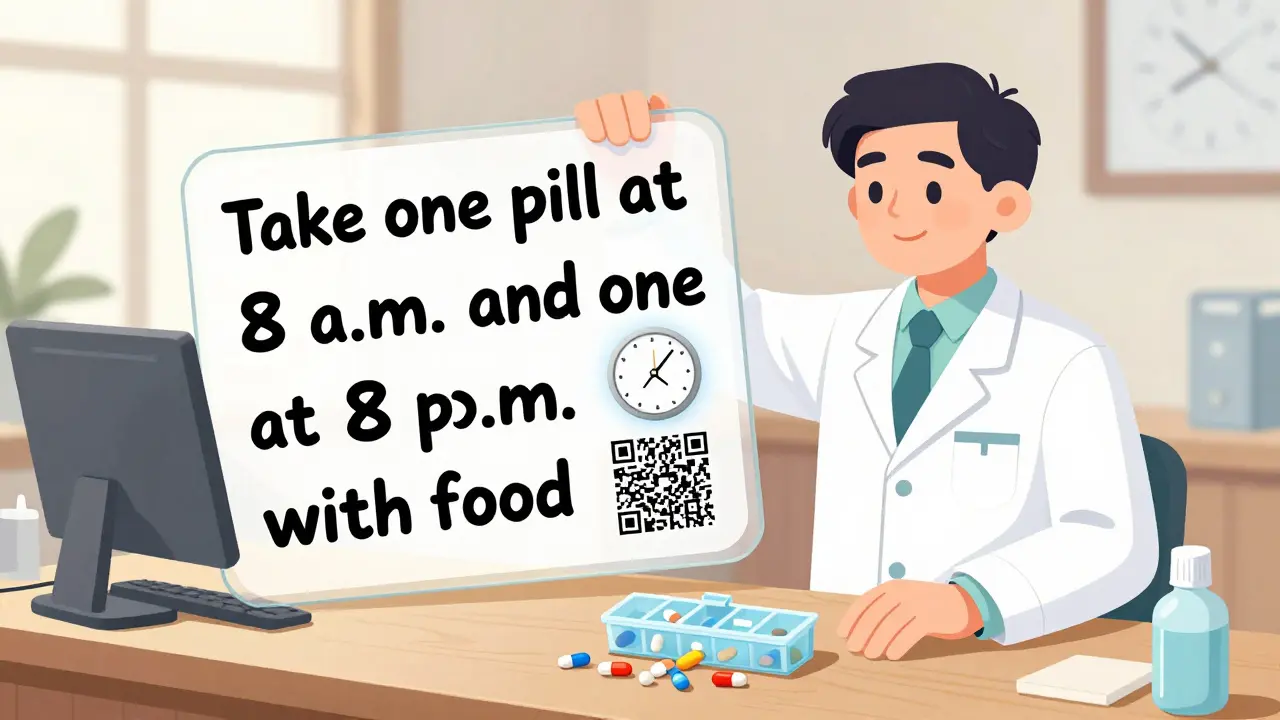
- Icons that actually make sense: a clock showing 8 a.m. and 8 p.m. next to "take twice daily."
- Large print options: available at 89% of major pharmacy locations.
- QR codes: scanning one links to a short video showing how to take the medicine.
These changes aren’t just nice-they work. In pilot programs, labels with clear instructions and visuals cut misunderstandings by 62%. The U.S. Pharmacopeia (USP) set standards for this back in 2007, but only 78% of chain pharmacies follow them. Independent pharmacies? Only 32% do. Why? Because updating software costs $2,500 to $5,000 per location.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s how to protect yourself:
- Ask the pharmacist to explain it in plain language. Say: "Can you tell me exactly when and how to take this?" Don’t let them rush you.
- Use the "Teach-Back" method. After they explain, say: "So, just to make sure I got it-I take one pill at 8 a.m. and one at 8 p.m., with food, right?" If they say yes, you’re good. If they hesitate, ask again.
- Request a large-print or translated label. If you’re not a native English speaker, ask for a Spanish, Chinese, or other language version. Only 12% of U.S. pharmacies offer this-but you can still ask.
- Take a photo of the label. Use your phone to snap a picture. Then use an app like GoodRx’s "Label Lens" to translate the instructions into plain English. It’s free and works 89% of the time.
- Write it down. Use a sticky note or your phone’s notes app. Write: "Take 1 pill at 8 a.m. and 8 p.m. with breakfast and dinner. Do not take on empty stomach."
- Use a pill organizer. 78% of people who use one say it helps them avoid mistakes. Buy one at any pharmacy for under $10.
Why This Matters More Than You Think
Medication errors cost the U.S. healthcare system over $500 billion a year. Nearly a third of that comes from simple label misunderstandings. That’s money spent on ER visits, hospital stays, and long-term damage that could’ve been avoided.
It’s also personal. Older adults, non-English speakers, and people with low literacy are hit hardest. One Medicare survey found 39% of seniors skipped doses because they didn’t understand the instructions. Another study showed Spanish-speaking patients were 3.2 times more likely to be confused by translated labels-because the translations were poorly done, not because they didn’t understand English.
But here’s the good news: when labels are clear, errors drop by 75%. That’s not a guess. That’s data from real studies at Mayo Clinic, Kaiser Permanente, and other top hospitals.

The Future of Prescription Labels
Change is coming. The FDA is considering making clear labeling mandatory by 2025. The Biden administration just allocated $200 million to improve health literacy in prescriptions. Amazon Pharmacy now offers voice-enabled labels-you can ask your phone to read the instructions out loud.
And technology is catching up. Apps like Label Lens can scan your label and rewrite it in simple language. Some pharmacies are testing smart pill bottles that beep when it’s time to take your medicine. These aren’t sci-fi-they’re here, and they’re working.
But until then, you’re your own best defense. Don’t assume the label says what you think it says. Don’t be shy about asking. Don’t guess. And if something doesn’t make sense, it probably isn’t meant to be understood that way.
What does "take with food" really mean on a prescription label?
It means you should take the medication while you’re eating or right after you finish a meal. This helps reduce stomach upset for certain drugs like antibiotics or pain relievers. It doesn’t mean "take it only if you’re eating" or "take it instead of food." If you’re unsure, ask your pharmacist to show you an example.
Why do some labels say "BID" or "QID" instead of "twice daily" or "four times daily"?
These are old medical abbreviations that pharmacists and doctors still use out of habit. "BID" means "bis in die"-Latin for twice a day. "QID" means "quater in die"-four times a day. But patients rarely know what they mean. Clear labels avoid these terms entirely and use plain English instead. You can always ask your pharmacist to translate them.
Can I ask for a bigger font on my prescription label?
Yes. All major pharmacies-CVS, Walgreens, Walmart-are required by law to offer large-print labels for free. Just ask at the counter. Many also offer labels in other languages. Don’t assume they’ll offer it-ask. It’s your right.
What should I do if I accidentally took my medicine wrong?
Call your pharmacist immediately. They’re trained to handle these situations and can tell you if you’re at risk. If you’re having symptoms like nausea, dizziness, or chest pain, go to the ER. Never wait to see if you "feel okay." Even small mistakes with certain medications can cause serious harm.
Are there apps that can help me understand my prescription label?
Yes. GoodRx’s "Label Lens" app lets you take a photo of your label and gets a plain-language explanation in seconds. It’s free, works offline, and has been tested by UCSF with 89% accuracy. Other apps like Medisafe and MyTherapy also help track doses and explain instructions. Download one before your next refill.
Final Tip: Don’t Guess. Ask.
Prescription labels aren’t designed to be puzzles. They’re meant to keep you safe. If you’re confused, you’re not stupid-you’re just dealing with a system that hasn’t caught up to real people. Ask questions. Write things down. Use your phone. Bring someone with you to the pharmacy. And remember: no question is too simple. Your life depends on getting this right.
