Why combo pills cost way more than you think
You’re on two medications. Your doctor hands you a prescription for a combo pill - one tablet that does the job of two. It sounds convenient. But here’s the catch: that one pill might be costing you 10 times more than buying the two generic versions separately.
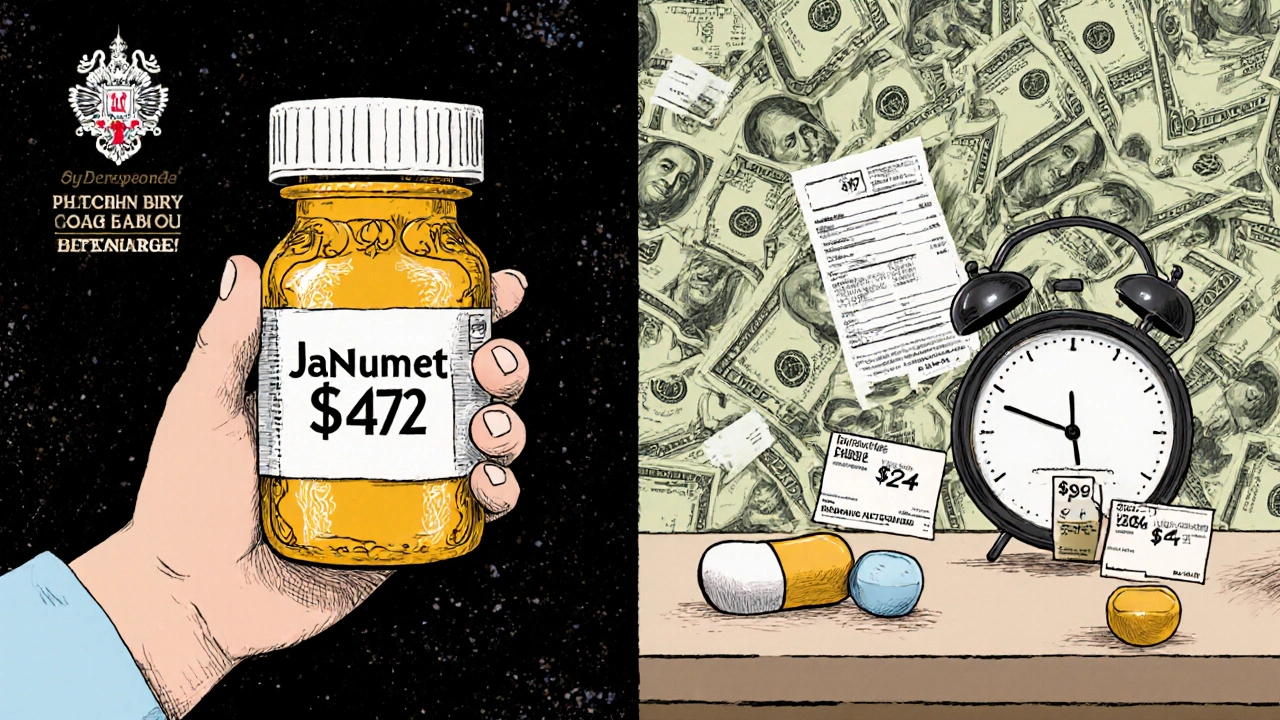
Take Janumet, a combo drug for type 2 diabetes. It combines sitagliptin and metformin. The branded version costs Medicare Part D about $472 for a 30-day supply. Meanwhile, generic metformin? At Walmart’s $4 program, it’s $4. The sitagliptin component? You can get it as a separate generic for under $20. Put them together, and you’re looking at roughly $24 for the same effect. That’s not a savings. That’s a $450 overcharge.
This isn’t an outlier. A 2018 study in JAMA Internal Medicine found that in 2016 alone, Medicare spent $925 million more on 29 branded combo drugs than it would have if doctors had just prescribed the generic versions separately. That’s $925 million wasted because patients and insurers were told the combo was better - even when it wasn’t.
How combo drugs work - and why they’re priced like luxury items
Fixed-dose combination (FDC) drugs are exactly what they sound like: two or more active ingredients in one pill. They’re common for conditions like high blood pressure, diabetes, HIV, and heart failure. The idea? Fewer pills, better adherence. And for some people, that’s true. But the pricing? That’s where things get strange.
Pharmaceutical companies don’t price combos based on cost. They price them based on what the market will bear. And here’s the trick: if one of the ingredients is still under patent, the whole combo gets treated like a brand-new drug - even if the other ingredient has been generic for years.
Take Nexlizet, a cholesterol drug. One component, ezetimibe, has been generic for over a decade. The other, bempedoic acid, is new and expensive. But because they’re in one pill, the whole thing gets priced like a breakthrough. In the U.S., it costs about $12 a day. Generic ezetimibe? Less than 20 cents a day. You’re paying for convenience - and a patent loophole.
This is called “evergreening.” It’s when drugmakers take old, cheap drugs, slap them together with a new one, and reset the clock on pricing. The FDA approves it. Medicare pays for it. Patients are stuck with the bill.
The math doesn’t add up - here’s what you’re really paying
Let’s break down the numbers. When two generic drugs are combined into one pill, the cost should be roughly the sum of both - maybe a little more for the packaging. But that’s not how it works.
According to IQVIA, branded combo drugs typically cost about 60% of what two separate branded drugs would cost. Sounds good, right? But when you compare them to generics, the gap explodes.
Here’s a real example:
- Entresto (sacubitril/valsartan) - branded combo: $580/month
- Generic valsartan: $12/month
- Sacubitril (brand only): $500/month
- Actual cost if bought separately: $512
Entresto costs more than the sum of its parts. And that’s not a mistake - it’s the business model.
Compare that to Kazano (alogliptin/metformin): $425/month for the combo. Generic metformin? Under $10. Alogliptin? Around $150. Total if bought separate: $160. That’s a $265 monthly markup. For a pill that does the same thing.
And here’s the kicker: 90% of all prescriptions in the U.S. are filled with generics. But combo drugs? They’re the exception. In 2021, combo drugs made up just 2.1% of prescriptions but 8.3% of Medicare Part D spending. That’s a massive imbalance.

Why doctors still prescribe them - and when it actually makes sense
If the math is so bad, why are combo pills still everywhere?
Because for some patients, they work better. Adherence matters. If you’re supposed to take four pills a day and you forget one, your blood pressure spikes. Your heart gets stressed. You end up in the ER. A single pill that you remember to take? That’s worth something.
Studies show combo pills improve adherence by 15-25% compared to multiple separate pills. That’s real. For elderly patients, people with complex regimens, or those with memory issues, a combo can be life-changing.
But here’s the difference: convenience isn’t the same as cost-effectiveness. A combo pill might help you take your meds - but it shouldn’t bankrupt you to do it.
And not all combos are created equal. If both ingredients are generic, the combo might cost only slightly more than the sum of the two. But if one is still under patent? That’s when the price jumps. And that’s when you should ask your doctor: “Can I get these separately?”
What you can do - and how to save hundreds a month
You don’t have to accept the price. Here’s how to fight back:
- Check your prescription. If it’s a combo drug, look up the two ingredients. Search for their generic names. Use GoodRx, SingleCare, or your pharmacy’s price checker.
- Ask your doctor. Say: “I found the generic versions of both drugs cost way less. Can I take them separately?” Most doctors are open to it - especially if you’re paying out of pocket.
- Check your plan’s formulary. Many Medicare Part D plans require prior authorization for combo drugs. If yours does, you might be able to get the generics approved instead.
- Use pharmacy discount programs. Walmart, Costco, and CVS have $4 or $10 generic lists. You can often get both drugs for under $20 a month.
- Ask about patient assistance. Some drugmakers offer co-pay cards - but read the fine print. Some only work if you’re on the brand, not the generic.
One patient in Oregon switched from Janumet to separate generics. Her monthly cost dropped from $472 to $26. That’s $5,358 saved in a year. She didn’t lose any effectiveness. She just stopped overpaying.
The bigger picture - why this keeps happening
This isn’t just about you. It’s about how the system is built.
Medicare Part D can’t negotiate drug prices directly. Private insurers have less leverage than the VA, which pays 22-33% less for the same drugs. So when a combo drug comes out, the price sticks - even when generics are available.
The Inflation Reduction Act of 2022 tried to fix this. It lets Medicare negotiate prices for some high-cost drugs. But combo drugs? They’re still mostly excluded unless both components are expensive. And even then, the process is slow.
Meanwhile, drugmakers keep filing new patents, tweaking dosages, and combining old drugs with new ones. The market for combo drugs is projected to hit $185 billion by 2027. Most of that growth will come from cardiovascular and diabetes meds - the exact places where generic alternatives already exist.
This isn’t innovation. It’s exploitation.

When you should stick with the combo - and when to push back
Not every combo is a rip-off. Here’s when to keep it:
- You’re on a complex regimen and forget pills often.
- Your doctor has tried separate meds and they didn’t work well together.
- You have kidney or liver issues and need precise dosing only available in the combo.
- Your insurance covers the combo at a low co-pay - and the generics cost more with your plan.
And here’s when to push back:
- One ingredient is generic and cheap.
- The combo costs more than the sum of the two generics.
- You’re paying out of pocket or have a high deductible.
- You’re not having any side effects or adherence issues with separate pills.
Don’t assume the combo is better. Ask for the data. Ask for the price. Ask for the option.
Final thought: Your health shouldn’t cost a fortune
Pharmaceutical companies aren’t evil. But the system is broken. And you’re paying the price - literally.
You deserve to take your meds without worrying about whether you can afford them. You deserve to know that the pill in your hand isn’t being priced to maximize profit, but to maximize your health.
Next time you get a combo prescription, don’t just fill it. Ask. Compare. Negotiate. You might save hundreds - or even thousands - without changing a single thing about your treatment.
Are combo pills always more expensive than buying two separate generics?
Not always - but in most cases where one ingredient is still under patent, yes. If both drugs are generic and available separately, the combo might cost only slightly more. But if one component is still branded, the combo often costs 10x more than buying the two generics together. For example, Janumet costs over $470/month, while generic metformin and sitagliptin together cost under $25.
Can my doctor prescribe the generic versions instead of the combo?
Absolutely. Doctors can and often do prescribe separate generic medications instead of combo pills. Many patients do this successfully, especially if they’re already used to taking multiple pills. The key is to ask. Your doctor may assume you want the combo, but they’re usually happy to switch if it saves you money.
Why do insurance plans cover combo drugs if they’re so expensive?
Insurance plans cover combos because they’re approved by the FDA and listed as standard treatments. Many plans don’t actively compare prices between combos and generics unless they’re flagged as high-cost. Some require prior authorization, which gives you a chance to appeal and request generics. But unless you push back, the combo gets filled by default.
Do combo pills really improve adherence?
Yes, studies show patients are 15-25% more likely to take their meds consistently when they’re in one pill. That’s especially true for older adults or people with multiple conditions. But this benefit doesn’t justify paying 10x more - especially when the same adherence can be achieved with pill organizers, reminders, or simpler regimens.
What’s the difference between a combo drug and a generic combo?
A combo drug is any pill with two or more active ingredients. A generic combo means both ingredients are off-patent and available as generics. Generic combos are rare because most combo drugs include at least one branded ingredient. When they do exist, they’re usually much cheaper - sometimes under $30/month. But they’re not always available, and pharmacies may not stock them.
Is there a law that stops drug companies from overcharging for combos?
Not directly. The Inflation Reduction Act lets Medicare negotiate prices for some high-cost drugs, but combo drugs are often excluded unless both ingredients are expensive. The FDA and CMS don’t regulate combo pricing - they only approve safety and effectiveness. That means the pricing gap between combos and generics is a market failure, not a legal one.
What to do next
If you’re on a combo drug, take 5 minutes today. Look up the two ingredients. Search their generic prices. Call your pharmacy. Compare the cost of the combo vs. the two separate generics. If there’s a big difference - talk to your doctor. You’re not asking for a favor. You’re asking for a fair price.
That $472 pill? It might be $26 with a simple switch. And that’s not just smart. It’s your right.