When you’re on treatment for osteoporosis, waiting a year or two to see if your bones are getting stronger can feel like gambling with your health. Bone density scans (DXA) are the gold standard, but they’re slow. That’s where bone turnover markers come in-giving you real-time feedback on whether your medication is working, often within weeks, not years.
What Are Bone Turnover Markers?
Bone isn’t static. It’s constantly being broken down and rebuilt-a process called remodeling. When bone breaks down (resorption), fragments of collagen spill into your blood and urine. When new bone forms (formation), proteins are released. These fragments and proteins are bone turnover markers (BTMs). They’re like smoke signals from your skeleton, telling doctors how active your bone remodeling is.
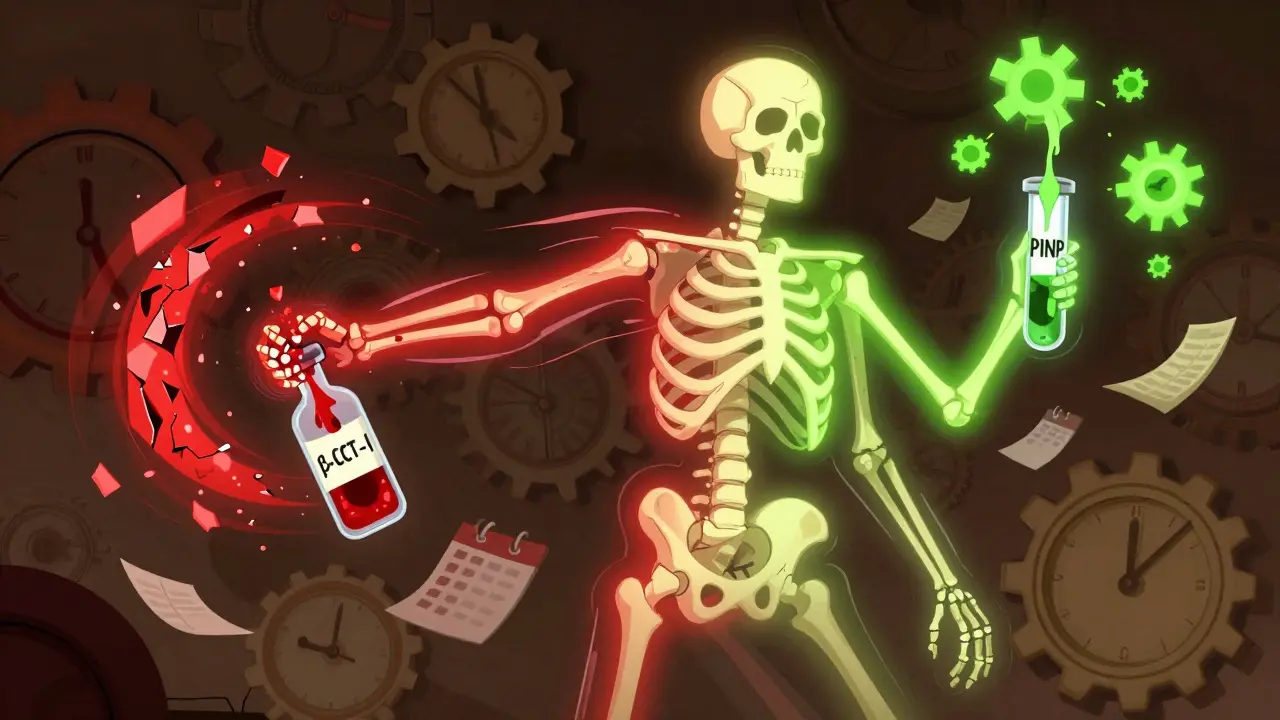
There are two main types:
- Resorption markers: Show how fast bone is being broken down. The most reliable is β-CTX-I (beta-C-terminal telopeptide of type I collagen), measured in plasma.
- Formation markers: Show how fast new bone is being made. The top choice here is PINP (procollagen type I N-terminal propeptide), measured in serum.
These two-PINP and β-CTX-I-are now the international standard, backed by the International Osteoporosis Foundation and European Calcified Tissue Society. Other markers like osteocalcin or urinary NTx exist, but they’re less precise or more affected by things like food intake or time of day.
Why Use Them Instead of Just Waiting for DXA Scans?
DXA scans measure bone mineral density, but they’re like taking a yearly photo of your house. You won’t know if the foundation is being repaired until the walls look stronger-months or years later. BTMs are like a motion sensor inside the walls. They tell you if repairs are happening right now.
Here’s the key difference:
- DXA scan: Detects changes in bone density after 12-24 months. Precision error: 1-3% at spine, 3-6% at hip.
- Bone turnover marker: Shows change in bone activity within 3-6 weeks. You can see if a drug is working by month 3.
For example, if you start a bisphosphonate (like alendronate or zoledronic acid), your β-CTX-I levels should drop by at least 30% within 3-6 months. If they don’t, your body isn’t responding. That’s not a failure of the drug-it might mean you’re not taking it correctly, or your body metabolizes it differently. Either way, you find out early.
For anabolic drugs like teriparatide (Forteo), the opposite happens: PINP levels jump 70-100% in the first few months. That spike tells doctors the drug is stimulating new bone growth. No waiting. No guessing.
How Doctors Use BTMs in Practice
The best approach isn’t to replace DXA-it’s to use BTMs to guide it. Here’s the standard protocol:
- Before starting treatment: Get a baseline BTM test. This gives you a starting point.
- At 3 months: Repeat the test. Did PINP drop by 35% or more? Did β-CTX-I drop by 30% or more? If yes, you’re on track. If not, your doctor can investigate why.
- At 12-24 months: Get a DXA scan to confirm actual bone density gains.
Why 3 months? Because that’s when the body responds to the drug. A 2022 study called TRIO showed patients who hit the 30% drop in β-CTX-I by month 3 had a 1.6% lower fracture risk after just 22 weeks. That’s a real-world benefit-not just lab numbers.
And here’s the kicker: BTMs can catch non-adherence. If your levels don’t change, but you say you’re taking your pills, something’s off. Maybe you’re swallowing your bisphosphonate with coffee. Maybe you’re skipping doses. BTMs don’t lie.

What Can Mess Up the Results?
BTMs are sensitive. If you don’t prepare right, the numbers can be wrong-even if your bones are fine.
For β-CTX-I:
- You must fast overnight (8-12 hours).
- Sample must be taken between 8-10 a.m. (CTX levels rise after meals and drop at night-up to 40% variation if you’re late or ate breakfast).
- Don’t drink alcohol or exercise hard the day before.
For PINP:
- Less affected by food, but still best taken in the morning.
- Diurnal variation is only 10-15%, so timing matters less than with CTX.
Also, some labs use different machines. A result from one lab might not match another. That’s why it’s best to use the same lab for all your tests. And not all labs follow the international standards-only about 65% in the U.S. do.
Who Should Get Tested?
Not everyone needs BTMs. But they’re most helpful for:
- People starting antiresorptive drugs (bisphosphonates, denosumab)
- People starting anabolic drugs (teriparatide, abaloparatide)
- Patients with poor adherence history
- Those with kidney disease (CKD stages 3-5)-standard markers like PINP and CTX can be skewed by poor kidney function, so bone alkaline phosphatase (BALP) or TRACP5b are better here
- Patients on long-term therapy where doctors want to know if they still need medication
For someone just diagnosed and starting treatment, BTMs give peace of mind. For someone on meds for 5 years, they can help decide if it’s safe to take a drug holiday.

Limitations and What BTMs Can’t Do
BTMs aren’t magic. They don’t tell you where your bone is weak. They don’t replace DXA. And they’re not perfect.
- Biological variability: Normal day-to-day fluctuation can be 20-60%. That’s why you need a 20-25% change to count as real.
- Population differences: Most reference ranges are based on white, European populations. Asian women often have 15-20% lower baseline CTX. African populations show higher PINP. Labs need to adjust for this.
- Cost and access: Medicare covers PINP (CPT 83970) and β-CTX-I (CPT 83935), but many private insurers still don’t. Out-of-pocket cost: $30-$40 per test.
- Not for diagnosis: You can’t diagnose osteoporosis with BTMs. Only DXA can do that.
Think of BTMs as a speedometer-not a GPS. They tell you how fast you’re going, not where you’re headed. You still need DXA to know if you’re getting closer to your destination.
The Future: Personalized Bone Health
The next wave is BTM-guided treatment. Imagine this: your doctor adjusts your dose or switches your drug based on your 3-month BTM result-not a guess, not a calendar date, but your body’s real response.
Trials are already underway. One study (NCT04567821) is testing whether using BTMs to guide therapy reduces fractures more than standard care. Another (NCT04892345) is looking at BTMs in postmenopausal women with early osteoporosis.
Point-of-care tests are also in development-think finger-prick tests you could do in your doctor’s office. If they get FDA clearance, BTMs could become as routine as a cholesterol test.
Experts agree: bone turnover markers are no longer experimental. As Professor Jean-Yves Reginster says, “The time has come for bone turnover markers to take their place as routine clinical tools.”
If you’re on osteoporosis treatment, ask your doctor: “Can we check my bone turnover markers at 3 months?” It’s a simple blood test. It could save you months of uncertainty-and maybe even prevent a fracture.
What are the best bone turnover markers for monitoring osteoporosis treatment?
The two most reliable markers are serum PINP (procollagen type I N-terminal propeptide) for bone formation and plasma β-CTX-I (beta-C-terminal telopeptide of type I collagen) for bone resorption. These are recommended by the International Osteoporosis Foundation and European Calcified Tissue Society as the reference standards due to their precision, stability, and strong correlation with treatment response.
How soon can I see changes in bone turnover markers after starting treatment?
Significant changes in bone turnover markers can be detected as early as 3-6 weeks after starting treatment, with clear results typically visible by 3 months. This is much faster than DXA scans, which require 12-24 months to show measurable changes in bone density.
Do I need to fast before a bone turnover marker test?
Yes, if you’re being tested for β-CTX-I, you must fast for at least 8-12 hours and have the blood drawn between 8-10 a.m. to avoid large fluctuations caused by food intake and daily rhythms. PINP is less affected by meals, but morning collection is still recommended for consistency.
Can bone turnover markers replace DXA scans?
No. DXA scans measure actual bone mineral density and are the only test approved for diagnosing osteoporosis. Bone turnover markers show how active your bone remodeling is, but they don’t tell you the current strength of your bones. They’re best used together-BTMs for early response, DXA for long-term confirmation.
What if my bone turnover markers don’t change after 3 months?
If your β-CTX-I doesn’t drop by at least 30% or your PINP doesn’t rise by 70-100% (for anabolic therapy), it could mean you’re not taking your medication correctly, your body isn’t absorbing it, or you’re on a drug that doesn’t suit your biology. Your doctor may check your adherence, adjust your dose, or switch your treatment. Non-response is a signal-not a dead end.
Are bone turnover marker tests covered by insurance?
Medicare covers both PINP (CPT code 83970) and β-CTX-I (CPT code 83935) for osteoporosis monitoring. Many private insurers now follow suit, but coverage varies. Out-of-pocket costs are typically $30-$40 per test. Always check with your provider before testing.
Can people with kidney disease use bone turnover markers?
Standard markers like PINP and β-CTX-I can be elevated in chronic kidney disease due to reduced clearance, making them unreliable. For patients with CKD stages 3-5, bone alkaline phosphatase (BALP) or TRACP5b are preferred alternatives. Reference ranges for these markers in kidney patients are still being refined, so testing should be done in specialized labs.