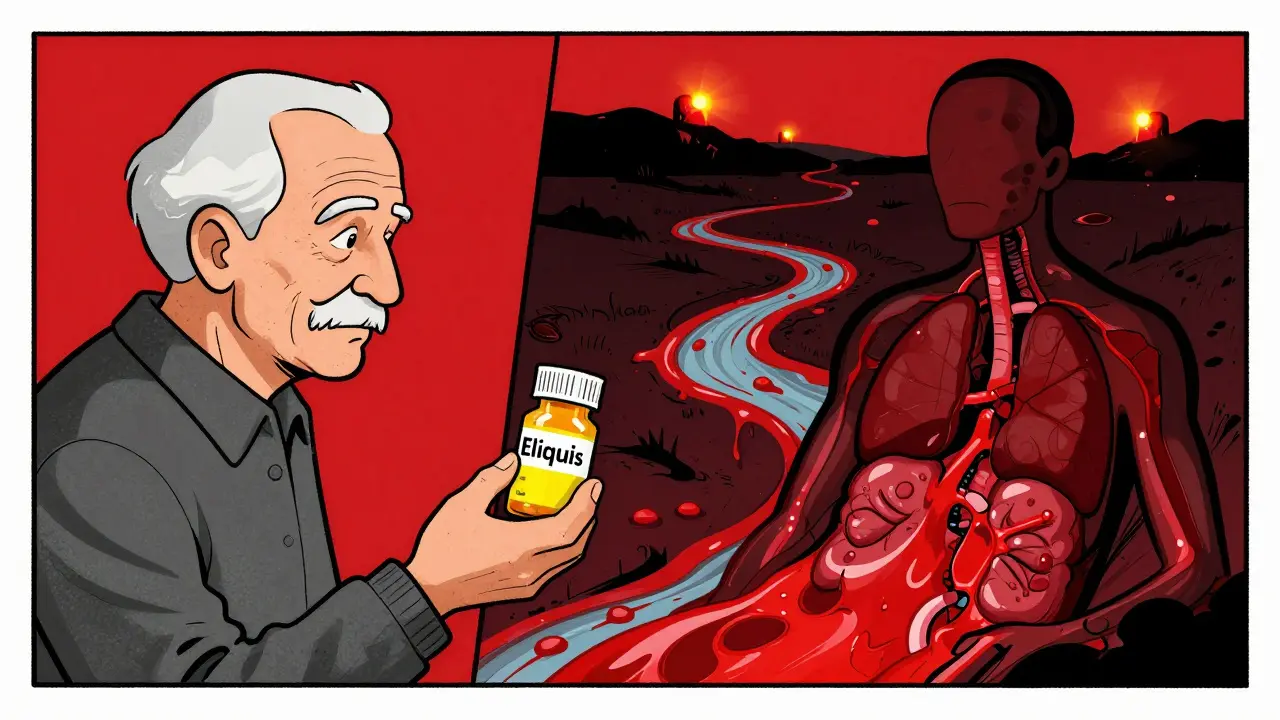
When you take a blood thinner, you're balancing life and death. These medications stop deadly clots from forming in your heart or brain, but if you take too much-or if your body reacts unexpectedly-they can start bleeding inside you without warning. And once internal bleeding starts, every minute counts. This isn't theoretical. In 2022, over 33,000 Americans ended up in the emergency room because of blood thinner overdoses. Many didn’t realize what was happening until it was too late.
What Happens When a Blood Thinner Goes Wrong
Blood thinners like warfarin (Coumadin), apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) work by slowing down your blood’s ability to clot. That’s good when you have atrial fibrillation or a replaced heart valve. But if your dose is too high, or you accidentally take two pills, your body can’t stop bleeding-even from tiny injuries. Internal bleeding doesn’t always show up as a cut or bruise. It can happen in your brain, stomach, kidneys, or muscles, and you might not feel it until you’re in serious trouble.Warfarin, the oldest and still most commonly used blood thinner, affects vitamin K, which your liver needs to make clotting proteins. When you overdose on warfarin, those proteins drop slowly. Your INR (a blood test that measures clotting time) might not spike right away. It can take 12 to 24 hours to rise, and the danger can last for days. Even if you feel fine, your body could be quietly bleeding.
Direct oral anticoagulants (DOACs) like Eliquis and Xarelto act faster and wear off quicker, but they’re just as dangerous in overdose. Unlike warfarin, they don’t need regular blood tests, which makes it easier to miss the warning signs. A 2023 study found that nearly 30% of people who ended up in the ER with DOAC-related bleeding didn’t realize their symptoms were connected to their medication.
Signs You’re Bleeding Inside
Internal bleeding doesn’t always scream for help. It whispers. And most people ignore the whispers until it’s too late.Here’s what to watch for:
- Black, tarry stools or blood in your stool-this means bleeding in your stomach or intestines.
- Pink, red, or dark brown urine-signs of bleeding in your kidneys or bladder.
- Coughing or vomiting blood, or material that looks like coffee grounds-this is upper GI bleeding, often from ulcers.
- Unexplained bruising-especially large bruises that show up without injury.
- Small red or purple dots under your skin-called petechiae-these are tiny bleeding spots.
- Prolonged bleeding from minor cuts, nosebleeds, or gum bleeding that won’t stop after 10 minutes of pressure.
- Heavy menstrual bleeding-soaking through a pad or tampon every hour.
- Severe headache, dizziness, confusion, or weakness-could mean bleeding in the brain.
- Sharp pain in your abdomen, back, or chest-could signal bleeding in your organs or around your spine.
One Reddit user, u/WarfarinWarrior, thought his dark stools were from eating beets. By the time he went to the ER, his hemoglobin had dropped to 6.2 g/dL (normal is 12-16). He needed a blood transfusion and spent a week in the hospital. He wasn’t alone. In a 2022 survey by the National Blood Clot Alliance, 62% of people admitted they ignored early symptoms because they thought it was "just a stomach bug" or "too much alcohol."
What to Do Right Now
If you suspect an overdose or see any of these signs, don’t wait. Don’t call your doctor’s office. Don’t check your phone for answers. Call 911 or go to the nearest ER immediately.Here’s what to do while you wait for help:
- Stop taking your blood thinner. Do not take another dose, even if you think you missed one.
- Don’t take NSAIDs. No ibuprofen, aspirin, naproxen, or even baby aspirin. These make bleeding worse.
- Write down what you took. Name of the drug, dose, time you took it, and how much you think you took. Bring the pill bottle if you can.
- Lie down and stay calm. Movement can make bleeding worse. Elevate your legs if you feel dizzy.
- Apply pressure to external bleeding. Use a clean cloth and press hard for at least 10 minutes. Don’t peek.
Don’t try to treat this at home. Vitamin K or reversal agents like idarucizumab or andexanet alfa are not available over the counter. They require hospital equipment, IV access, and monitoring. Even if you feel okay now, your INR could climb hours later.
How Doctors Treat It
Emergency treatment depends on what drug you took and how bad the bleeding is.For warfarin overdose without active bleeding but with an INR above 4.5, doctors give you oral vitamin K-usually 1 to 5 mg. If you’re actively bleeding, they give you 4-factor Prothrombin Complex Concentrate (PCC), which replaces the missing clotting factors fast. They’ll also give you IV vitamin K to keep working for days. Fresh frozen plasma (FFP) is used if PCC isn’t available, but it’s slower and can overload your heart.
For DOACs, things are simpler if you have the right reversal agent. If you took dabigatran (Pradaxa), they’ll give you idarucizumab. If you took apixaban or rivaroxaban, they’ll use andexanet alfa. These drugs work in minutes. But they’re expensive-up to $10,000 per dose-and only available in hospitals.
For recent overdoses (within 1 hour), doctors may give you activated charcoal to stop the drug from absorbing. But if it’s been more than 60 minutes, charcoal won’t help. And no, drinking milk or eating food won’t fix it.
What Happens After
If you survive, you’ll need close follow-up. Your INR will be checked daily until it’s stable. You might need to switch to a different blood thinner, or your dose will be lowered. Some people never take anticoagulants again after a major bleed.Long-term, you’ll need a bleeding risk checklist. Keep it on your fridge or phone. Check it every day:
- Any new bruising?
- Any blood in urine or stool?
- Any unusual headaches or dizziness?
- Any bleeding that lasts longer than 10 minutes?
- Any pain in your belly, back, or head?
Patients who use point-of-care INR monitors-devices you can use at home for $200-$300-have 34% fewer major bleeds, according to a 2022 study. If you’re on warfarin, ask your doctor if one is right for you.

Why This Keeps Happening
The CDC says anticoagulant errors are the second most common serious medication mistake in adults over 65. Why? Because these drugs are complex, and patients aren’t trained to spot the signs.Doctors often assume patients know what to watch for. But most don’t. A 2023 survey found that only 18% of people on warfarin could name three signs of internal bleeding. Even worse, 41% said they didn’t know if their INR was in range.
That’s why the FDA requires every blood thinner box to have a black box warning-the strongest safety alert. But warnings don’t help if you don’t read them. Or if you forget.
One fix? Keep a simple log. Write down your dose every day. Use a pill organizer with alarms. Tell a family member what you’re taking. If you’re over 65, ask your pharmacist to review all your meds-many blood thinner overdoses happen because of drug interactions with antibiotics, painkillers, or even herbal supplements like ginkgo or garlic.
What’s Coming Next
There’s hope on the horizon. In 2023, the FDA approved a new drug called ciraparantag for Phase III trials. It’s a universal reversal agent-meaning it can stop bleeding from any blood thinner, including DOACs and heparin, in under 10 minutes. If it works, it could cut ER wait times and save thousands of lives.But until then, your best defense is awareness. Know your drug. Know your signs. Know what to do when things go wrong.
Can I just take vitamin K at home if I think I overdosed?
No. While vitamin K reverses warfarin, it takes hours to days to work. If you’ve overdosed and are bleeding, you need immediate clotting factors from PCC or other hospital treatments. Taking vitamin K alone can delay life-saving care. Always call 911 first.
Do all blood thinners cause the same kind of bleeding?
The symptoms are similar-internal bleeding looks the same no matter the drug. But the timing differs. Warfarin’s effects build slowly and last days. DOACs like Eliquis work fast and wear off in 12-24 hours. That means DOAC overdose symptoms can appear quickly, but also resolve faster if caught early. Still, both require emergency care.
Is it safe to take aspirin with a blood thinner?
Never take aspirin, ibuprofen, or naproxen with a blood thinner unless your doctor specifically says so. These drugs thin your blood further and can turn a small bleed into a life-threatening one. Even low-dose aspirin can be dangerous. Always check with your doctor before adding any new medication.
Can I drink alcohol while on blood thinners?
Moderate alcohol (one drink a day) is usually okay, but heavy drinking raises your bleeding risk and can make warfarin levels unstable. Alcohol also irritates your stomach lining, which can trigger GI bleeding. If you drink regularly, tell your doctor. You may need more frequent INR checks.
What should I do if I miss a dose of my blood thinner?
If you miss a dose, take it as soon as you remember-but only if it’s within a few hours. Never double up the next day. If it’s been more than 6-8 hours, skip the missed dose and take your next one at the regular time. Doubling up increases overdose risk. Always check your drug’s specific instructions or call your pharmacy.
Are there any foods I should avoid with warfarin?
Yes. Vitamin K-rich foods like kale, spinach, broccoli, and Brussels sprouts can make warfarin less effective. You don’t need to avoid them completely-just keep your intake consistent. Sudden changes in your diet can throw off your INR. Talk to your doctor or dietitian about a stable meal plan.
How often should I get my INR checked?
When you first start warfarin, you’ll need weekly checks. Once stable, it’s usually every 2-4 weeks. If your INR keeps swinging, you may need checks every week. Patients who use home INR monitors can test themselves weekly and reduce hospital visits. Ask your doctor if home testing is right for you.
