Asthma and COPD both make breathing hard, but they’re not the same thing. Many people mix them up because they cough, wheeze, and feel short of breath. But the causes, how they progress, and how they’re treated are completely different. Getting the right diagnosis isn’t just about labels-it changes your life. One can be controlled with daily meds and few flare-ups. The other slowly damages your lungs for good. If you’re over 40 and have breathing trouble, or if your child wheezes every spring, knowing the difference matters.
What Happens Inside Your Lungs
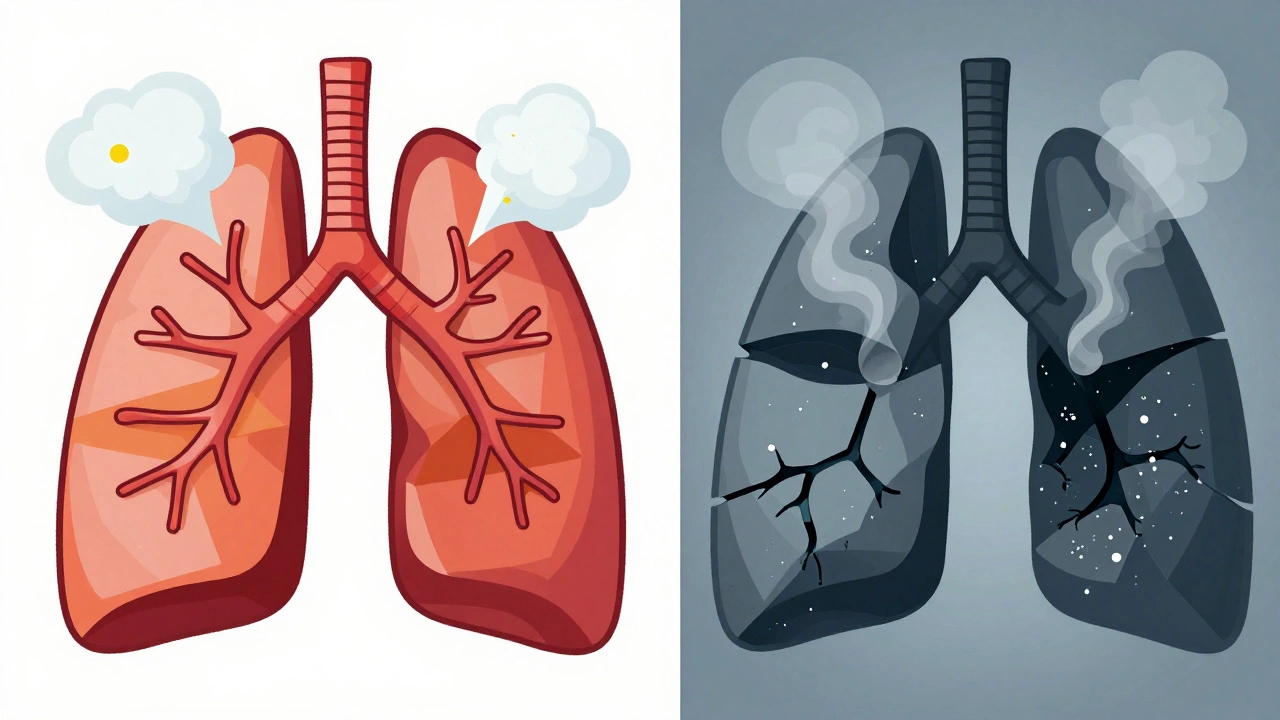
Asthma is like a sensitive airway that reacts too hard to triggers. Allergens, cold air, exercise, or stress can make the muscles around your airways tighten, swell up, and fill with mucus. The good news? That narrowing usually goes away-on its own or with an inhaler. Your lungs don’t get permanently damaged. Most people with asthma have stretches where they feel totally normal.
COPD is different. It’s not a reaction-it’s a breakdown. It’s usually from years of smoking or long-term exposure to fumes and dust. The air sacs in your lungs (alveoli) get destroyed in emphysema. In chronic bronchitis, the tubes get swollen and clogged with thick mucus. This damage doesn’t heal. Your lungs lose elasticity. Air gets trapped. You’re always breathing harder, even on good days.
Symptoms: When It’s Flare-Ups vs. Constant Struggle
If your symptoms come and go, asthma is more likely. You might wake up at 3 a.m. wheezing after a party with lots of perfume, or get winded after climbing stairs during a cold snap. Between episodes, you feel fine. A dry cough is common. You probably don’t spit up much phlegm.
COPD doesn’t take days off. You have a daily cough that brings up mucus-often yellow or green. You’re out of breath just getting dressed. By the time you’re diagnosed, you’ve been ignoring it for years. You might notice your lips or fingernails turning slightly blue when you’re tired-that’s low oxygen. You don’t have allergy seasons. You have bad days, every day.
Who Gets It and When
Asthma often starts in childhood. Half of all cases are diagnosed before age 10. It’s common in kids with eczema or hay fever. Family history matters-a lot. If one twin has asthma, the other has a 70% chance of getting it.
COPD rarely shows up before 40. Nine out of ten people diagnosed are over 45. The biggest risk? Smoking. About 90% of COPD cases are linked to cigarettes. Even if you quit decades ago, the damage sticks. Non-smokers can get it too-from long-term exposure to wood smoke, pollution, or workplace dust-but it’s rare.
How Doctors Tell Them Apart
Pulmonary function tests are the gold standard. You blow into a machine that measures how fast and how much air you can push out. In asthma, your numbers improve dramatically after using a rescue inhaler-usually a 12% or bigger jump in FEV1. That’s reversibility. It’s a clear sign your airways are still responsive.
In COPD, that number barely moves. Even after the inhaler, your airflow stays stuck. That’s because the damage is structural, not just tight muscles.
Another tool: fractional exhaled nitric oxide (FeNO). If your breath has more than 50 ppb of nitric oxide, it means your airways are inflamed with eosinophils-the kind tied to allergies and asthma. COPD patients usually test under 25 ppb.
Blood tests help too. Eosinophil counts above 300 cells/μL point toward asthma or overlap syndrome. Below 100? Likely pure COPD. High-resolution CT scans show emphysema in 75% of COPD patients. In asthma? Only 5% show those changes.
Treatment: Different Goals, Different Tools
Asthma treatment is about control and prevention. Start with a rescue inhaler (albuterol) for quick relief. If you’re using it more than twice a week, you need a daily anti-inflammatory-usually an inhaled corticosteroid. For severe cases with high eosinophils, biologic shots like mepolizumab can cut flare-ups by half.
COPD treatment is about slowing decline and managing symptoms. First-line meds are long-acting bronchodilators-either LABAs or LAMAs. These relax airways all day. Steroids? Only if you’re having frequent flare-ups. You won’t get biologics-they don’t work for COPD’s type of inflammation.
Pulmonary rehab helps COPD patients more than asthma patients. After 8-12 weeks of exercise and breathing training, COPD patients can walk 54 meters farther in six minutes. Asthma patients? Maybe 12 meters. Why? Because their lungs weren’t broken to begin with.
The Overlap: ACOS
One in five people with obstructive lung disease has something called Asthma-COPD Overlap Syndrome (ACOS). These patients have features of both. They might have had asthma since childhood, then smoked for 20 years. Now they have a chronic cough, mucus, and still wheeze after allergens.
ACOS is tougher to treat. They have more flare-ups than either condition alone-almost twice as many as asthma patients. Doctors often use triple therapy: two long-acting bronchodilators plus an inhaled steroid. But evidence is still growing. No one knows yet if this is the best long-term strategy.

Prognosis: Life Expectancy and Quality of Life
Asthma patients who manage their condition well have a 92% chance of living 10 more years. Most die from other causes-heart disease, cancer-not asthma.
COPD is more serious. Even moderate cases drop survival to 78% over 10 years. Hospitalizations happen more often-almost once a year on average. Each flare-up speeds up lung decline.
Quitting smoking changes everything for COPD. People who stop cut their disease progression by half. For asthma, smoking doesn’t make it worse unless it’s mixed with COPD. But if you have asthma and smoke, you’re way more likely to develop COPD later.
What You Should Do Now
If you’re wheezing or short of breath:
- Track your symptoms. Do they come and go? Or are they always there?
- Do you have allergies, eczema, or a family history of asthma?
- Have you smoked-or been around smoke for years?
- Do you cough up mucus every morning?
See a doctor. Get a spirometry test. Don’t assume it’s just “bad lungs” or “aging.” Misdiagnosis is still common-1 in 4 people over 40 with breathing problems are told the wrong thing.
And if you smoke? Quit now. No matter what you’re diagnosed with, stopping smoking is the single most powerful thing you can do to protect your lungs.
Can asthma turn into COPD?
Not directly. Asthma doesn’t become COPD. But if you have asthma and smoke for many years, you can develop COPD on top of it. This is called ACOS-Asthma-COPD Overlap Syndrome. It’s not one disease turning into another. It’s two diseases coexisting. About 15-25% of people with obstructive lung disease have this mix.
Is COPD curable?
No. COPD causes permanent damage to the lungs. You can’t reverse it. But you can slow it down. Quitting smoking, taking prescribed meds, doing pulmonary rehab, and avoiding lung irritants can help you breathe better and live longer. The goal isn’t a cure-it’s managing the disease so it doesn’t control your life.
Can I use my asthma inhaler for COPD?
Short-acting rescue inhalers like albuterol are safe to use for both conditions during sudden breathing trouble. But daily control meds are different. Asthma patients often use inhaled steroids every day. COPD patients usually don’t-unless they have frequent flare-ups. Using the wrong meds long-term won’t help and could cause side effects. Always follow your doctor’s plan, not someone else’s.
Why do I need a spirometry test if I already feel like I have asthma?
Because symptoms can be misleading. Many people think wheezing equals asthma. But COPD can also wheeze. So can heart failure or vocal cord dysfunction. Spirometry measures actual airflow. It shows if your airways are reversible (asthma) or fixed (COPD). Without this test, you might get the wrong treatment-and your condition could get worse.
Does having asthma mean I’m more likely to get COPD?
Only if you smoke. Asthma alone doesn’t increase your risk for COPD. But if you have asthma and you smoke, your risk goes up dramatically. Studies show smokers with asthma are four times more likely to develop COPD than non-smokers with asthma. The combination of inflamed airways and smoke damage creates a perfect storm for lung destruction.
Are biologic injections only for asthma?
Yes-for now. Biologics like omalizumab and mepolizumab target specific immune cells (eosinophils) that drive allergic asthma. These don’t work in typical COPD because the inflammation is different-it’s from smoke, not allergies. But in ACOS patients with high eosinophils, some doctors use them off-label. Research is ongoing, but they’re not FDA-approved for COPD or ACOS yet.
What’s Next?
If you’ve been told you have asthma or COPD, ask for your spirometry results. Ask about your eosinophil count. Ask if you need a CT scan. Don’t accept a label without proof.
If you’re still smoking, talk to your doctor about quitting programs. Even one less cigarette a day helps. If you’re using your rescue inhaler more than twice a week, it’s time to adjust your treatment.
And if you’re a parent and your child has frequent wheezing-don’t wait. Early diagnosis and proper asthma control can prevent lifelong problems. Most kids outgrow it. But only if it’s managed right.